DO YOU know a practice owner who wants more patients in her clinic, better pay-per-visit, and better collections? We all know healthcare practice owners who want to remain independent and grow and yet are frustrated by insurance companies and continuous battles to get paid and stay compliant.
Now, as a patient, do you like visiting a healthcare practice, receiving bills, and reconciling them with your insurance company? You are not alone. As it turns out, most other people do not like their patient experience.
The problem is that patient and independent practice needs have evolved in step with society and technology, but management methodology remained in the 19th century. There’s a fundamental mismatch between how healthcare practices and patients are managed — and the practice owners’ and patients’ expectations.
We came to a startling observation: patients no longer want their care to be managed the way it used to be managed in the previous century. And yet, practice owners still use their old methods to memory-manage their practice. Who is taking advantage of this mismatch? The insurance companies – payers.
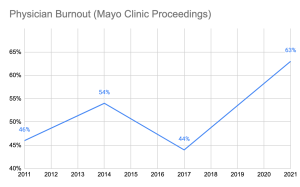
From the outset, we knew that healthcare costs are spiraling out of control. We also knew that insurance companies, medical equipment manufacturers, pharmaceuticals, and hospital executives have been all making handsome returns and benefitting from healthcare cost growth. One question bothered us: why are the practice owners unable to participate in that growth? How was it that the key contributors to healthcare service were excluded from fair compensation for their work and grew exceedingly frustrated with rules and regulations? Some providers were selling their practices to join larger networks or hospitals, and others were moving to different industries. National studies have shown that physician burnout rates are climbing up. For instance, Mayo Clinic Proceedings reported that the prevalence of burnout among U.S. physicians was 63% in 2021, compared with 38% in 2020, 44% in 2017, 54% in 2014, and 46% in 2011.
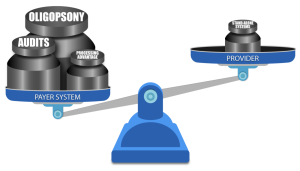
We also noticed that with experience, medical billing managers start cherry-picking insurance companies for easy follow-up. So, the practice owners could not get paid on time and in full by a growing number of insurance companies (payers). The more obstacles payers pose – the less paid the providers are. Payers were stacking the game against the providers by continuously adding new rules to reduce payments and increasing the frequency of provider audits.
In addition to continuous consolidation, resulting in scarcity of payers (a market structure known in economics as Oligopsony), which allows the payers to drive the reimbursement fees down, they also have a two-pronged resource advantage:
- attract Ivy-league MBAs to build sophisticated claim-processing protocols and discover every little pretext to deny or delay claim payment
- leverage the most powerful digital technology to implement those protocols on the ever-growing volume of claims.
ClinicMind was founded to address two basic challenges facing providers: a patient-provider expectations mismatch and payer-provider adversity. First, the patients have transformed how they expect healthcare service delivery, but practice owners have not adapted their practice management methodology. Second, insurance payers underpay and delay payments because they make a substantial profit from the “float.” The float is the money insurers hold onto between the time they collect premiums and the time they pay out claims.
In summary,
1. The Basic Mismatch Between Patients and Providers:
a. Background:
The healthcare industry has undergone significant changes in recent years, with patients becoming more proactive in managing their healthcare and demanding a different level of service. This transformation is largely due to increased access to health information through the Internet and the rise of patient-centered care models. However, many practice owners, particularly in traditional healthcare settings, have not adapted their practice management methodology to meet these changing patient expectations.
b. Conflict:
- Patient Expectations: Patients today expect convenience, transparency, and a more personalized approach to healthcare. They want to schedule appointments online, access their medical records easily, and receive timely, clear communication from their healthcare providers.
- Provider Resistance: Many practice owners and healthcare providers are accustomed to traditional, paper-based methods and may hesitate to embrace digital technologies or change their established processes. This resistance can result from the comfort with the status quo, fear of the unknown, or high implementation costs.
c. Resolution:
- To resolve this conflict, healthcare practices must adapt to the changing landscape. This may involve investing in electronic health records (EHR) systems, online appointment scheduling, telemedicine services, and more. Additionally, training staff and providers to use these technologies effectively is crucial.
- Clear communication with patients about these changes, the benefits they bring, and how data security and privacy are maintained can help build trust and reduce resistance.
2. Payer-Provider Adversity:
a. Background:
In the healthcare system, insurance payers (such as health insurance companies) often maintain a substantial portion of their profit through a financial mechanism called the “float.” The float is the money insurers hold onto between the time they collect premiums and the time they pay out claims. This float can represent a significant source of income for payers. However, it can create a conflict of interest with healthcare providers.
b. Conflict:
- Payer Profit: Insurance payers benefit from maintaining a healthy float, as they can invest these funds and earn returns. The larger the float, the more profit they can potentially make. Payers have a significant advantage over the providers because of the oligopsony and because of significantly larger resources for better talent hiring and data processing.
- Provider Concerns: Healthcare providers, on the other hand, often face challenges in receiving timely and appropriate payments from payers. Delays or disputes in claims processing can impact their cash flow and ability to provide care. Providers feel that payers prioritize maintaining their float over ensuring prompt reimbursement.
c. Resolution:
- Transparency and fair contracting: Establish clear and fair contracts between payers and providers that outline payment terms, including prompt payment schedules and dispute resolution mechanisms.
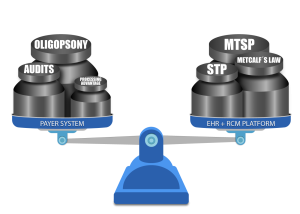
- Industry consolidation: Metcalf’s Law states that the value of a network is proportional to the square of the number of connected users or devices in the network. First, providers can gain negotiation power against the payers by consolidating into larger provider networks or joining hospitals. Next, providers also gain economies of scale, which can be applied to hiring better billing services, access to superior computing power, and administrative costs savings.
- Leverage of Modern EHR and RCM Platforms: Providers can control office chaos, improve billing efficacy, and reduce waste by leveraging diverse multi-faceted software systems integrated on a Multi-Tenant Single Platform (MTSP) and effective services built using Straight-Through Processing (STP) methodologies.
In both conflicts, open communication, adaptation to changing circumstances, and provider’s access to adequate computing power and services can help mitigate the challenges and ensure that healthcare is delivered effectively and efficiently. The healthcare industry is evolving, and all stakeholders need to work together to meet the changing needs of patients and providers while maintaining financial sustainability.
References
- Tait D. Shanafelt, et al, “Changes in Burnout and Satisfaction With Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic,” September 13, 2022, https://www.mayoclinicproceedings.org/article/S0025-6196(22)00515-8/fulltext
- Fred Bazzoli, Burnout by the numbers, February 22, 2023, https://www.healthdatamanagement.com/articles/burnout-by-the-numbers
A Future Book Publication Note:
This article is a chapter in the forthcoming 2nd Edition book “Medical Billing Networks and Processes,” authored by Dr. Yuval Lirov and planned for publication in 2024. We will post more chapters on this blog soon.