ClinicMinders make our company what it is. We hire for practice service aptitude over experience and pride ourselves on attracting and retaining people with COURAGE.
COURAGE to stick to our Core Values and help providers remain independent and grow. We also believe in radical transparency, so we publicly share Core Values with anyone who is interested in our approach to work. This fanatical focus is more than a mantra; it is evident in our software, the support we provide, and the services we keep adding. And doing so makes us ecstatic.
ClinicMind offers great benefits, an attentive team, and a flexible and professional work environment
ClinicMind offers a work-from-home (WFH) employment structure for work-life balance and professional growth. WFH benefits promote job satisfaction, family focus, and productivity.
ClinicMind leverages its access to the global talent pool and fosters a strong remote company culture through adherence to the core values of excellence, learning, and teamwork.

We are a Health IT and RCM service company with a leading-edge EHR software product and a medical billing BPO. We are looking for an enthusiastic Client Support Specialist. This role involves a broad range of responsibilities, from responding to client inquiries to troubleshooting and beyond. The ideal candidate is a problem-solver, an effective communicator, and dedicated to enhancing user experience.
Responsibilities:
Client Assistance:
Guide ClinicMind clients in maximizing the system's utility.
Handle a wide array of inquiries, including but not limited to patient demographics, balance management, clinic reporting, claims, and point of sale.
Problem-Solving:
Troubleshoot issues encountered by users.
Understand the objectives behind users’ actions and identify any obstacles they may face.
Inquiries and Training:
Address basic medical billing questions after completing mandatory on-the-job training.
Collaboration:
Work closely with our software support and account management teams to resolve client issues effectively.
Determine when an issue needs to be escalated to other departments for resolution.
Communication:
Engage with clients through various channels, including phone, email, live chat, Facebook, and an internal tasking system.
Escalation and Risk Management:
Identify practices at risk of attrition and escalate to the appropriate resource.
Recognize tone, keywords, and signs of frustration to address client concerns proactively.
Administrative Duties:
Ensure accurate documentation of all client interactions.
Follow up on client interactions as per established procedures.
Additional Responsibilities:
Perform other duties as assigned by management, adhering to the dynamic needs of the department.
Qualifications:
Proven experience in customer support or a similar role.
Excellent problem-solving and analytical skills.
Strong verbal and written communication abilities.
Ability to work effectively in a team and independently.
Familiarity with medical billing processes is a plus.
Proficiency in using various communication platforms including live chat and social media.
Commitment to providing high-quality support to enhance client satisfaction.
Position Requirements:
Must have stable internet connection minimum of 5 MBPS
Must have a mobile data plan as a backup
Must be in a quiet environment
Must be comfortable working the US business hours
Must own a PC with at least 8 GB of memory
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, seeks a Financial Modeling and Valuation Analyst. The successful candidate will be responsible for building financial models to support organic and inorganic corporate growth initiatives. If you are a self-driven individual with a passion for finance and a strong attention to detail, we want to hear from you.
Key Responsibilities:
Develop and maintain financial models to support strategic decision-making related to company growth opportunities
Analyze financial data and trends to provide insights and recommendations to senior management
Collaborate cross-functionally with various teams to gather information and input for accurate financial modeling
Support M&A activities by conducting due diligence, financial analysis, and valuation modeling
Monitor and evaluate financial performance against key performance indicators
Prepare and present financial reports and presentations to senior leadership
Qualifications:
Proficiency in Excel or Google Sheets, including working with Macros and financial modeling software
Experience in a corporate setting (not just academic) in the following:
Interpreting financial statements.
Interpreting historical company information.
Interpreting and analyzing company operations data to feed into the financial model.
Building financial models.
Building Discounted Cash Flow (DCF) models.
Building financial models by forecasting revenue and costs.
Performing scenario analysis against the models.
Preparing reporting of KPIs based on the financial model planned versus actual data.
Knowledge of the following:
Business valuation techniques.
Cost of capital valuation.
Dashboard and data visualization techniques
Preferred:
Candidate who has worked on financial analysis in one of the following environments: investment banking, venture capital, or private equity.
Must Have:
Experience with IT companies, preferably SaaS
High comfort level working on Eastern Time Zone/US Shift
Good internet access at home at least 25 MBPS
Mobile Hotspot
Laptop/Desktop of at least 16 GB
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, is looking for an Enrollment Specialist. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
We are seeking a detail-oriented and proactive Payer Enrollment Specialist to join our team. The Payer Enrollment Specialist will be responsible for managing the enrollment process with various healthcare payers, ensuring ensuring seamless integration of EDI and ERA services, and enabling efficient claims submission, payment processing, and reconciliation.
Key Responsibilities:
1. Managing EDI and ERA Enrollment Process
EDI Enrollment: Facilitate the enrollment of healthcare providers for EDI services with various payers, ensuring seamless electronic data exchange for claims submission and processing.
ERA Enrollment: Oversee the enrollment process for Electronic Remittance Advice (ERA), ensuring that providers receive electronic payment and remittance advice from payers.
2. Communication and Coordination
Liaison with Payers: Communicate with insurance companies to obtain necessary forms and documentation for EDI and ERA enrollments, ensuring timely submission and activation of services.
Internal Collaboration: Coordinate with internal departments to gather required information and documentation from providers and streamline the enrollment process.
3. Record Maintenance and Monitoring
Enrollment Tracking: Maintain accurate records of EDI and ERA enrollments, including submission dates, activation status, and any communication with payers.
Monitoring Activation: Monitor the activation of EDI and ERA services for providers, ensuring successful implementation and troubleshooting any issues that may arise.
4. Compliance and Reporting
Regulatory Compliance: Stay informed about EDI and ERA enrollment requirements, regulations, and industry standards to ensure compliance with payer guidelines.
Documentation and Reporting: Ensure all documentation related to EDI and ERA enrollments is completed accurately and in accordance with payer specifications, and generate reports as needed
Qualifications:
Bachelor's degree in any STEM domain (preferred) or medical doctorate
More than 1 year of Previous experience in payer enrollment, specifically with a focus on Electronic Data Interchange (EDI) and Electronic Remittance Advice (ERA) enrollments.
In-depth understanding of EDI and ERA enrollment processes, including familiarity with EDI transaction sets (such as ANSI X12) and ERA formats (such as ANSI 835).
Proficiency in using EDI enrollment tools and platforms, with experience in submitting EDI enrollment forms and managing EDI setup processes.
Strong communication and interpersonal skills, with the ability to effectively liaise with insurance companies and internal stakeholders to facilitate enrollment activities.
Excellent organizational skills and attention to detail, with the ability to maintain accurate records of enrollment activities and monitor enrollment status.
Knowledge of regulatory requirements and industry standards related to EDI and ERA enrollments, including HIPAA regulations and payer-specific enrollment guidelines.
Ability to work independently and prioritize tasks in a fast-paced environment, with a proactive approach to problem-solving and troubleshooting.
Proficiency in Microsoft Office applications, with experience in generating reports and analyzing enrollment data.
MUST HAVE:
High comfort level working on Eastern Time Zone/US Shift
Good internet access at home at least 25 MBPS
Mobile Hotspot
Laptop/Desktop of at least 16 GB
ClinicMind is a leading healthcare technology company providing comprehensive practice management solutions, including EHR software and medical billing services. Our mission is to streamline administrative tasks, improve clinical outcomes, and enhance the overall patient experience. Join us in revolutionizing healthcare through innovative digital solutions.
We are seeking a highly-skilled, self-reliant Senior Product UX Designer to join our dynamic team. This role is critical in shaping the future of our products through exceptional user-centered design. In this role you will also be a key contributor in building and maintaining our design system, mentoring other designers, and elevating our team’s capabilities. If you are passionate about creating impactful digital experiences, thrive in a collaborative environment, and have a keen eye for both design and product strategy, ClinicMind is the perfect place to advance your career.
Responsibilities
Product Design Leadership: Lead the design of new features and improvements across our product suite. Ensure designs align with product strategy and user needs.
User Research & Discovery: Engage with stakeholders to understand workflow shortcomings, pain points, and user needs. Conduct interviews, surveys, and usability tests to gather insights.
Data Analysis & Strategy: Analyze data to identify areas for improvement and propose solutions. Develop user personas, use cases, customer journey maps, and user flows.
Design Execution: Create low-fidelity and high-fidelity prototypes that address user needs and business goals. Ensure designs are consistent with ClinicMind’s branding and style guidelines.
Stakeholder Engagement: Present design concepts and prototypes to stakeholders, gather feedback, and iterate on designs to meet requirements and expectations.
Design System Management: Lead the development, documentation, and maintenance of our design system. Ensure consistency and scalability across all products.
Mentorship: Mentor and guide junior designers, fostering a collaborative and growth-oriented team environment. Provide feedback and support to enhance the team’s overall design capabilities.
Minimum Qualifications
Experience: At least 5 years of experience in UX design, including designing web user interfaces and experience with EHR UI is a plus.
Tools: Proficiency in Figma and other industry-standard design tools.
Knowledge: Strong understanding of UX design principles, usability, and technology limitations. Experience with design systems and creating design assets (vector, icons, guides, etc.).
Communication: Excellent verbal and written communication skills in English.
Education: Bachelor’s degree in Design, Computer Science, or a relevant field.
Portfolio: Must submit a portfolio showcasing relevant UX design work and demonstrating experience in designing user interfaces for web, mobile, or other digital products.
Preferred Qualifications
Knowledge of Material Design and its coding limitations.
Understanding of the US healthcare system.
Familiarity with HTML, CSS, and JavaScript.
NOTE
We seek a highly skilled and experienced Chief Mental Health Officer or Vice President of the Mental Health Division to lead the development and growth of a practice management solutions business in the psychiatric healthcare domain while leveraging the ClinicMind SaaS platform for Electronic Health Record (EHR) software and Revenue Cycle Management (RCM) service.
Responsibilities:
Develop and execute business strategies to drive revenue growth and market expansion for the mental health EHR software and RCM service business.
Identify and pursue new business opportunities to establish partnerships and collaborations with psychiatric and behavioral healthcare providers, healthcare organizations, and other relevant stakeholders.
Lead a team of product managers, sales and marketing professionals, and customer experience managers to achieve business goals and objectives.
Build relationships with key clients, affiliate partners, and stakeholders to drive business growth and customer satisfaction.
Lead the development of a mental health EHR software and RCM service business on top of the ClinicMind platform, including planning, designing, and implementing new features and functionalities.
Collaborate with cross-functional teams to ensure seamless integration with ClinicMind software and services.
Qualifications:
At least five years of experience in business development and managing operations expansion and development.
At least five years of experience in the behavioral health or psychiatric healthcare industry.
Proven track record of driving revenue growth and market expansion for software and services businesses.
Proven track record of managing multiple operations, marketing, and finance projects.
In-depth knowledge of mental health EHR software, RCM services, and healthcare industry trends and regulations.
Experience working with cross-functional teams and managing complex projects.
An advanced degree (e.g., a Master's or MBA) in mental health, healthcare administration, business, or a related field is preferred.
MUST HAVE:
Experience with IT companies, preferably SaaS
High comfort level working on Eastern Time Zone/US Shift
Good internet access at home at least 25 MBPS
Mobile Hotspot
Laptop/Desktop of at least 16 GB
ClinicMind is a Healthcare IT and Revenue Cycle Management (RCM) service company. We are looking for a full-time RCM Data Entry Associate, who enters billing process data, Demographics, Charge Entry and EOB / Cash Posting, Denial analysis and documentation.
Apply Now
RESPONSIBILITIES
QUALIFICATIONS
MUST HAVE:
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, is looking for a Senior Full Stack Java Developer. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
Apply Now
RESPONSIBILITIES
Participate in all phases of the software development life cycle
Develop new features and maintain and optimize Vericle EHR
Write well-designed, testable, efficient code
Build and debug modules in Java, GWT, GXT, and server-side Typescript
Web development in
Angular, Material Design
Backend work
Create/Maintain REST APIs
Develop, manage, and optimize Oracle queries
Develop, manage, and optimize MongoDB queries
QUALIFICATIONS
5+ years of experience
Java, Kotlin is a plus
Angular, HTML, CSS, JavaScript/Typescript
Oracle, PL/SQL, MongoDB
Source control
Bachelors in Engineering (Computer Science / B.Tech).
Must be able to adapt and learn to work within an unfamiliar codebase quickly
Must be a team player with excellent written and verbal communication skills
Bachelors in Computer Engineering or Computer Science
NOTE
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, is looking for a Senior Front End Software Developer. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
RESPONSIBILITIES
Build responsive web applications using Javascript, JQuery, CSS etc
Debug and fix issues
Enhance functionality and add new features
Convert mock UI designs into prototypes, creating excellent interactions from designs
Build a design for code structure, functionality, and organization
Profile and optimize inefficient code
Participate in code reviews, analyze peer performance, mentor junior developers
Build, enhance, evaluate, and/or incorporate tools such as build pipelines, unit test frameworks, code validation, and IDE plugins
QUALIFICATIONS
5+ years of experience
Full grasp of HTML, CSS, JavaScript, Typescript, and AJAX-based JSON/XML web services
Development experience in REST APIs, Angular, Material, Bootstrap
Source control
Solid foundation creating cross-browser and responsive web experiences
Understand the nuances of supporting tablet and mobile browsers
Must be able to adapt and learn to work within an unfamiliar codebase quickly
Must be a team player with excellent written and verbal communication skills
Bachelors in Computer Engineering or Computer Science
NOTE
ClinicMind is a leading company in providing Healthcare IT and RCM services, including EHR software and medical billing in the US. We are looking for a full-time Credentialing Specialist to help us keep growing. If you're excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
Apply Now
RESPONSIBILITIES
Handle credentialing needs for our clients (Group and/or Individual) who are US-based health care providers, diagnostic laboratories and medical facilities as preferred providers in health care networks. This entails the following tasks:
QUALIFICATIONS
MUST HAVE:
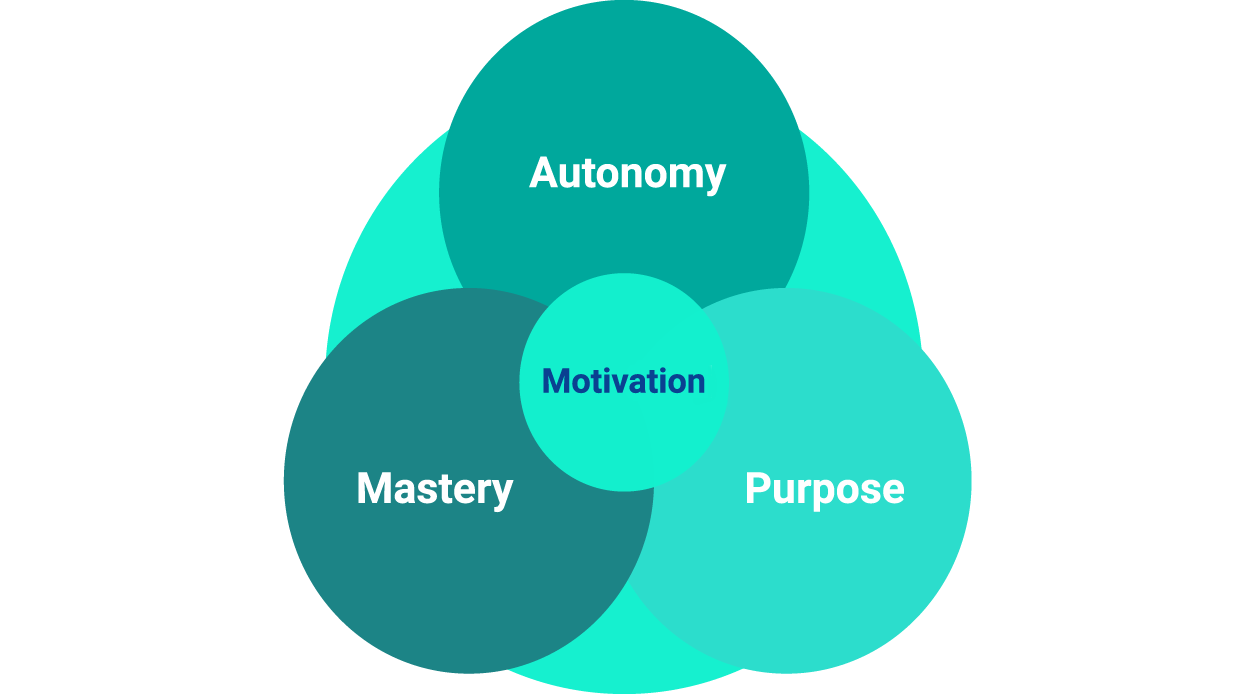
We strive for excellence throughout our hiring process.
We share the purpose of making a lasting change in the healthcare industry by building together state-of-the-art software and using it to level the playing field with the payers.
We invest our energies in learning and mastering our skills, and we grow our responsibilities in step with our professional and business growth.
This site includes cumulative user rating numbers, video testimonials, press releases, and other social proof materials across all brands and all resellers leveraging ClinicMind Software and/or Service as a Platform (SaaP). For more detail about our white labeling and reselling models, visit our About Page or Contact Us directly. Check Privacy Policy