The insurance industry operates on the principle of shared risk, meaning that while everyone pays in, only a fraction of those people will actually take something out. The difference between what’s paid in and what’s paid out is known as the financial float.
Properly managing the financial float is key to an insurance company’s profits. However, it is a complex equation influenced by inflation and the assessed risk of the insured population. It also factors into a major problem known as payor-provider adversity.
The Financial Float
Insurance companies generate profits by collecting premiums. In return for premiums, individuals are given peace of mind that they will be covered under certain circumstances. However, insurance companies know that only a small fraction of the insured population will truly file a claim, which is how they remain profitable.
In addition to managing risk based on whom they insure, insurance companies can also maximize profits by managing the “financial float.” The financial float is the difference between the premiums paid by the patient to the insurance company and the amount the insurance company pays to service providers.
It is the insurance company’s responsibility to maintain the value of the float, even as the value of the dollar drops from day to day. After all, policyholders expect services to be provided in accordance with their policy agreement, even if that agreement was made many months ago when a dollar was worth substantially more.
In order for insurance companies to fulfill their obligations and remain profitable, they must invest the premiums they receive. The longer the insurance company can commit each dollar to an investment, the higher their returns can be. This incentivizes the insurance company to hold on to the float for as long as possible, minimizing how much they pay out and delaying how quickly they pay out, thus posing a conflict of interest.
The Challenges Service Providers Face
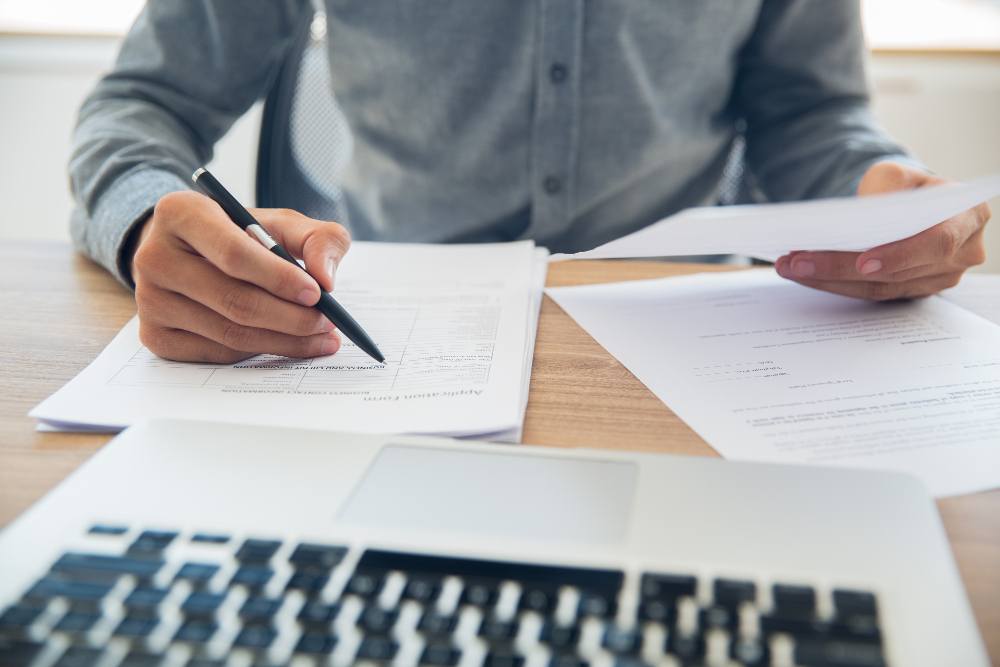
When service providers, such as hospitals and private practices, deliver services to a patient, they submit a claim to the patient’s insurance company on their behalf. Filing a claim requires complex documents including detailed information about the patient, provider, procedure, and the diagnosis that justified the procedure. For this reason, there are many opportunities for error.
Payers (i.e., insurance companies) must be extremely careful to identify errors, or else they could end up paying out on fraudulent claims. As a result, service providers must be extremely meticulous when filing claims to avoid errors that can lead to denied and delayed payments. When a claim is denied, payers are required to provide a reason, but it tends to be cryptic and not overly explicit. This means service providers must spend time deciphering the issue and find the missing or incorrect data so that they can resubmit. Due to the complexity, many private practice owners choose to hire a third-party company to handle their billing to ensure they are getting paid should any of these errors occur and avoid errors in the first place.
For service providers, having a claim go through the first time is important for a number of reasons. First and foremost, if they have too many claims flagged with government payers like Medicare or Medicaid, they could lose their license. Secondly, delayed and denied claims are extremely harmful to cash flow. Every time a claim is denied, the payment could be delayed by up to a few months, depending on how quickly the service provider can resubmit their claim and how quickly the payer processes it.
What’s more, payers are continuously reducing the reimbursement they pay to service providers for various services. This essentially means that service providers must seek out new patients and deliver a higher volume of services, which in turn leads them to spend more time on marketing and patient care. However, more patients mean more claims, creating a greater administrative burden and increasing the risk of error.
The Technological Advantage
On the payer side, claims processing is never done manually. Insurance companies have the finest resources available, hiring Harvard MBAs and other competent experts to create advanced processes capable of identifying errors quickly. They will then hire the best programmers to build solutions that flag errors accordingly and process them properly.
Truly, the only way for a provider to work at the same level of efficiency is to have a similarly powerful system, which is why the concept of “strength through billing” is gaining traction. Service providers can become extremely effective at filing claims and handling denials by implementing programs able to identify errors and suggest how to handle them. Of course, this software has its flaws.
While payers need only check claims documents, service providers must implement systems that aid in their creation. This means they require a fully integrated system capable of reducing administrative burden while capturing all of the critical details about a patient’s visit, diagnosis, and procedure.
ClinicMind is one such tool helping to streamline practice management without the rigidity that most digital solutions offer. It leverages data and AI systems created through the processing of over 72 million claims over the span of 20+ years. ClinicMind empowers physicians to customize the patient flow based on their habits and preferences so that things aren’t just faster, but also easier. For instance, practices can still enjoy the flexibility of handwritten notes with the freehand app, while also benefiting from the accessibility and traceability that comes along with digitizing those notes.
Using a solution like ClinicMind, practices are able to increase overall administrative efficiency so that they can worry less about filing claims and dealing with reimbursement delays and spend more time actually caring for patients. Ultimately, such a software solution does not make payer-provider adversity disappear, but it does level the playing field.
While payers and providers will continue to have opposing interests, service providers able to utilize the latest technology will no longer have to bolster their cash flow by taking on excessive patient loads or hiring additional claims professionals. Instead, they can ensure that they are collecting and tracking the right information with every patient visit to inform the claims process, reduce errors, and speed up the payment timeline.