AI for outcomes-based compensation in healthcare

What is outcomes-based compensation in healthcare? Compensation plans in the healthcare industry have undergone a paradigm shift, with more providers moving away from volume-based to outcome-based compensation for their employees. This is partly attributable to the rising healthcare costs and enhanced patient empowerment, with a growing need for better quality of service delivery (Zigrang, 2022). Volume-based models compensate providers for the quantity of care delivered rather than the impact on the health status of patients (Tai et al, 2014). The vision for outcomes-based compensation in healthcare revolves around incentivizing and rewarding healthcare providers based on the outcomes they achieve in patient care rather than just on the volume of services delivered. This approach aims to improve the overall quality of care, enhance patient outcomes, and reduce healthcare costs. However, existing literature on outcomes-based compensation models shows mixed results in terms of impacts on quality of care and costs, with some reporting significant cost savings and others reporting increased costs of care, as expounded later on in this chapter. In an outcomes-based compensation model in healthcare, providers are encouraged to focus on delivering measurable results and positive patient experiences. This may involve achieving specific health outcomes, such as reducing hospital readmission rates, improving patient satisfaction scores, or effectively managing chronic conditions. By aligning compensation with outcomes, healthcare organizations aim to drive better patient outcomes, ensure patient safety, and enhance healthcare delivery. Healthcare outcomes reflect the quality of care offered by practice and remain stable over time compared to process measures, which keep changing over time. For instance, the target outcomes in a diabetic care clinic include reduced blindness, reduced amputation rates, improved self-management and confidence, and reduced heart attacks. These target outcomes that matter to patients the most tend to remain stable over time regardless of where you practice. On the other hand, process measures such as fundoscopic examination, blood glucose assessment, foot care, and medication review may vary over time. This forms one of the basis for outcomes-based compensation models (Dunbar-Rees, 2018). The outcomes-based compensation model offers several benefits to different players in the healthcare field. Patients get to enjoy quality care over volume, with the potential to address health inequalities. This is so because the model emphasizes outcomes that matter to patients, which tend to remain constant regardless of the geographical location. For instance, the target outcomes for a diabetic care clinic in Kisumu, Kenya, Africa, would be more or less the same as for a clinic in Atlanta, Georgia, USA. For the providers, outcomes-based compensation helps reduce the wastage of resources and unnecessary interventions by enabling efficient resource allocation. It also reduces fragmentation of care by encouraging collaboration and coordination across clinicians and specialties. The payers benefit through reduced wasted healthcare spend as well as focusing on buying healthcare that is based on outcomes that matter most to their beneficiaries (World Economic Forum, 2023). The outcomes-based model has been implemented across different healthcare facilities worldwide in a bid to improve the quality of care and reduce costs. There are several studies showing the impact of outcomes-based models on the quality of care, resource utilization, and healthcare costs. These studies show varied outcomes, with some reporting positive impacts and others reporting negative impacts or no significant impacts. For instance, the Pioneer Accountable Care Organizations (ACO) implemented by the Center for Medicare and Medicaid Services in the USA as an outcome-based compensation model reported a reduction in healthcare costs by approximately $385M in two years compared to the previous volume-based compensation model, with no difference in quality of care (McCarthy, 2015). The Medicare Shared Savings Program, which was also designed to incentivize cost reduction, reported similar cost savings of $385M dollars over one year of implementation (Eijkenaar & Schut, 2015). However, some studies suggest that outcomes-based models were associated with additional healthcare costs, mainly in the form of bonuses and incentives paid out to healthcare workers. For instance, the Quality and Outcomes Framework (QOF) implemented in the UK as a pay-for-performance program was reported to have spent about US $9 billion on incentive payments over a period of just seven years (Ryan et al, 2016). Outcomes-based compensation models impact on the quality of care delivered to patients, albeit to varying extents from the available literature. In one study, the Quality and Outcomes Framework model operationalized in the UK to incentivize family practitioners for target patient outcomes resulted in an increase in the median practices achieving the target HbA1C levels for diabetic patients from 59% to 66.7% in two years. (Vaghela et al, 2009). However, another study evaluating the impacts of the same Quality and Outcomes Framework in the UK on hypertension reported no significant change in blood pressure monitoring rates and treatment intensity attributable to the program. There was no significant difference in the cumulative incidence of stroke, renal failure, and heart failure as well (Serumaga et al, 2011). With such mixed data on the impacts of pay-for-performance on costs and outcomes, it is evident that this alone may not be sufficient to improve the quality of patient care, and more factors need to be accounted for in order to achieve optimal patient care quality. Another study in rural Kenya evaluated the utility of outcomes-based compensation models in improving the management of suspected malarial fevers. The program rewarded measures of process quality of care, including the proportion of patients correctly given antimalarial drugs based on test results. Incentives were provided to facilities with increased rates of treatment for confirmed malaria cases, as well as those with reduced treatment rates without any confirmatory tests. From the study, the odds of receiving treatment following a negative malaria test in the intervention arm was 0.15 relative to baseline, compared to 0.42 in the comparison facilities that were not enrolled in the program. This translated to a 2.75 times greater reduction of inappropriate prescription of antimalarial drugs in the incentivized groups compared to the comparison groups (Menya et al, 2015). Another instance in which the outcomes-based model has been utilized is through Humana’s
What Does it Mean to be ONC Certified and Why Does It Matter?
In today’s digital age, technology has become a cornerstone of our daily lives, and this is particularly evident in the healthcare sector. Medical practices now require robust and secure methods for data management. Advanced Electronic Health Record (EHR) systems are pivotal in this regard, enabling the efficient exchange and management of patient information, as well as streamlining administrative tasks. The healthcare sector’s growth has prompted the Office of the National Coordinator for Health Information Technology (ONC) to define specific criteria for EHR systems. These criteria ensure that such systems are structured effectively to gain certification. EHR providers, including Genesis, have the option to submit their products for ONC’s evaluation and certification. Understanding ONC Certification The ONC’s Health IT Certification Program was initiated under the Public Health Service Act. This program aims to establish benchmarks within the rapidly evolving domain of health information technology. EHR systems undergo rigorous testing by independent third parties, focusing on their ability to record, secure, and share information. Certification is granted only to those systems that adhere to the ONC’s stringent standards. For medical practitioners, using an ONC-certified EHR system is essential to qualify for Medicaid and Medicare incentive payments. This certification also instills confidence in both healthcare providers and patients regarding the secure and efficient handling of health information. ONC’s Trusted Partners Accreditation Laboratories and Certification Bodies The ONC collaborates with a select group of laboratories for the certification process. Currently, these include: Drummond Group ICSA Labs InfoGard Laboratories, Inc. SLI Compliance, a Division of Gaming Laboratories International, LLC These labs, with their diverse expertise, including in healthcare, are responsible for the thorough testing and certification of EHR systems. For instance, Drummond Group, has successfully tested and certified Genesis under the 2015 Edition Health IT Module. Impact on Healthcare Professionals and Patients The involvement of independent laboratories in testing EHR software ensures that medical professionals are not solely reliant on the claims of service providers. Only EHR systems that meet the high standards of security, reliability, and functionality achieve ONC certification. This assures healthcare staff and physicians that their chosen software adheres to the highest Health IT standards. Adopting an ONC-certified EHR system also has financial benefits for medical practices. It enables them to avoid Medicare payment penalties and secure Medicaid incentive payments, while simplifying processes for both staff and patients. Patients, too, stand to gain from the widespread adoption of these certified systems. EHRs simplify healthcare management and enhance the security of personal health information, ensuring privacy and peace of mind.
Are You Someone’s Hero?
In the last chapter we talked about hunger and the drive that must exist between all members of a patient community, including the patients themselves, but what about the patient’s need for a mentor? Remember in previous chapters we talked about how Joseph and Bonnie’s dispositions not only affected their ability to treat effectively but also resulted in lost patients? Patients, because they are people, respond and react to the emotions they receive. We don’t always react in the expected way, but that has more to do with the person interpreting than the person reacting. So how do we set ourselves up so that when we aren’t having the best day ever and performing at our peak state, our patients still receive the best care possible? The answer is heroism. And no, I’m not talking about superhero heroism like we see in the movies today. I’m talking about the heroism of someone behaving in a consistent and positive way that inspires others. When people see someone working harder than everyone else (and I don’t mean slightly harder, I mean orders of magnitude harder), they naturally want to help that person. Following success is a tremendous motivator for many because it means that they don’t have to expect 100% effort from themselves to achieve a goal. In other words, the responsibility isn’t 100% on them, and so they feel compelled to work as hard as possible, if not harder. We all know the power of heroes in fiction and how they inspire their comrades and even enemies, in many cases, to follow the path of good and righteousness. Take the most famous superhero of them all. Superman. As we prepare for the dawn of the Superman movies in cinema, these films raise powerful questions about what is meant by a leader. Many would say that Superman is an example of a great hero, but I would disagree. Superman is a great character and, in fiction, does amazing things for many. However, because his power is so great and far removed from our own, we don’t feel like what he does is ever enough (hence people never truly appreciate Superman except when their lives are on the line). As practice owners and clinicians, we’re often seen this way. We hold in our minds and hands, the ability to create massive change in a patient’s life, change that that patient would otherwise be unable to experience. This truly defines us as Superheroes, but it also presents a major problem. It means we are too far removed from our patients resulting in this kind of detached relegation. We feel compelled as patients to receive care and do so reluctantly, hoping we never need to return (think about it, how many patients truly want to be thinking about their illness?). Now take the example of the practice owner and how we react when we feel like superheroes. Sure, at the beginning, it’s an incredible ego booster, it makes us feel like we are kings and invincible. But then what? The feeling goes away, and we’re left with a patient roster that, quite frankly, is embarrassing by superhero standards. Naturally, this gives way to the feeling of inadequacy and negativity we discussed earlier. So what do we need to do? Simple (but not easy), we need to get closer to our patients. In other words, we need to close as much of the rift between a patient and their physician as possible. Since this is a natural phenomenon with man-made side effects, it is especially difficult to resolve. It means that we, as practice owners, have to first overcome our confidence needs to see ourselves as our patients see each other, powerful and capable. Above is a diagram that describes what I’m talking about. Nature develops these build-in separations as we grow in expertise and capability, but it also creates a lack of empathy and connection with our patients. The real question is, who is responsible for bridging this gap? Heroism lies in effective communication with patients and addressing their concerns holistically. As a practitioner, you should be able to listen to, understand, and share in people’s feelings, beliefs and experiences in order to take care of their real needs and offer individualized care rather than just focusing on the science of the illness. This is part of the spectrum of empathetic communication (Moudatsou et al, 2020). Several strategies can be used to effectively communicate with patients. These include active listening, using plain language while avoiding technical jargon, using relatable examples and illustrations, using appropriate language, keeping the interaction confidential and letting patients explain concepts in their own words to demonstrate understanding. (Tulane University School of Public Health and Tropical Medicine. Strategies for Effective Communication in Health Care. Sept 2021; Float Care 2023 ) Here’s a great personal example. In graduate school, I was a teacher’s assistant (professor lackeys or TAs as we were widely known) teaching the recitation for a course on statistics for Psychology undergraduate majors. These were first-year students who, for the most part, had no idea what they were doing, but also knew exactly what they were doing. As with most young people, there was a split, and although they needed guidance, they weren’t ready to admit it yet. This was clear in the first month as I clearly entered the room as an authority figure. I was confident in my knowledge of the material and ability to convey it in a manner that would instruct students (sounds engaging, doesn’t it?). Obviously, you can imagine what happened next: I inspired exactly zero students to actually be interested in the material and as a result, many did not pass the first exam. There was an uproar from the professor and from the students, apparently thinking that the recitations were the source of the problem. The professor sat me down for an hour over coffee and tea (I was the difficult one who didn’t and still doesn’t drink coffee), explaining the difference between
Are You Hungry?

Great, now Reuven wants to know if I’m hungry. Don’t worry, we’re not talking about hunger pains or anything like that. I’m talking about drive, the hunger to stop at nothing to succeed. But I’m also not talking about it in the most general sense. In other words, we’re not talking about all those Youtube videos dealing with motivation, drive, and hunger. I’m talking about the hunger unique to healthcare that is required to create a thriving practice. I’m talking about community hunger. When you want to put together a thriving patient community, regardless of specialty, of course, it’s critical that both you, your staff, and your patients feel a certain hunger. Gone are the days of thriving practices where patients simply receive care. Today, a thriving practice depends on the teamwork built between a patient and the staff in the office. However, anytime you have a team, you need teamwork based on a voracious hunger. A driving force that unites the team and propels them forward. Clearing objectives, roles, and expectations; providing training and support; promoting diversity and representation; providing incentives and feedback; and securing institutional support and sponsorship are all examples of effective patient engagement tactics, according to a systematic review on the topic published in Bombard et al. (2018). One of the biggest misconceptions about hunger and drive is that you must be an extrovert or high-energy person to derive strength from hunger truly. In fact, I’ve quite often experienced the opposite. In Joseph and Bonnie’s case, these two had opposing personalities, but Bonnie, who was more of an introvert than Joseph’s incredible extroversion, was clearly overcome by a stronger hunger. She was more consistent in her behavior and suffered from less burnout than Joseph. She was also more adaptable. She was able to empathize with both high-energy patients and low-energy ones. Experience really is the best teacher, and more often, it’s easier to understand high-energy people from a low-energy perspective than to understand low-energy people from a high-energy perspective. According to research, personality factors have been linked to job satisfaction and burnout among healthcare professionals. For instance, higher neuroticism levels have been associated with lower job satisfaction, increased emotional exhaustion, and depersonalization. Contrarily, agreeability and scrupulosity are positively connected with job satisfaction and adversely associated with depersonalization (Kang & Malvaso, 2023). These findings imply that managing burnout and enhancing worker well-being in healthcare settings can be facilitated by understanding various personality types. I’ll give you a personal example. I am a high-energy person who loves to be loud, talk fast, and get from A to B with as little in between as possible. I was always the quintessential type A personality who never enjoyed the journey because he was too caught up in achieving the destination. In school, that can often do well for you, as I always achieved top scores on exams and papers. However, my personal relationships suffered greatly. For example, I could never maintain quality friendships (although I had many friends), and forget about romantic relationships where you truly need to be present to be successful. Imagine being so caught up in the result of effort and bringing that to a romantic situation. Strong leadership is crucial in community-based healthcare practices. Effective community involvement projects have been shown to involve communities in planning, designing, implementing, and evaluating primary health care services. Community leaders are essential in promoting teamwork and driving the group toward shared objectives (Erku et al., 2023). Ultimately, I had to recognize the drawbacks of my personality and the opportunities that presented. In other words, what were the challenges I had to overcome, and how would those help me to become a better and more contributing individual? At the same time, I struggled because some of my friends had great connections, and I often felt that they were lazy because they spoke slower, didn’t engage at a super high level of energy, and often stayed home instead of constantly going out. It’s important to consider the varied personality types’ needs for recharge time (Grailey et al., 2023). Now we understand the difference in recharge time required for different personality types. For example, if you are more introverted, you can definitely be the life of the party, but afterward, you’ll need some time to recharge the batteries. There’s nothing wrong with this; in retrospect, I think this is more beneficial than constantly being out. The literature also emphasizes the importance of reflection and self-awareness in identifying one’s fundamental limitations and comprehending the advantages associated with various personality characteristics. Extroverts may thrive in social situations and get their energy from continual engagement, but introverts have a special ability to use deep thought and reflection to advance both personally and professionally. This implies that accepting and comprehending one’s innate characteristics might result in personal growth and achievement in a variety of areas of life (Grailey et al., 2023). It challenges us to search for that hunger within instead of constantly being hungry for what’s outside of us. In my personal struggle to expand beyond my core limitations, I recognized the incredible power of introverted people and how I could leverage that to grow personally and professionally. However, one of the biggest mistakes people make is thinking they can grow this way independently. In other words, they think there is a way for them to simply absorb this information without help. Nothing could be further from the truth. Studies have underlined the value of mentoring for improving patient outcomes, career growth, and skills in healthcare settings (Nandwani, 2023). The analogy of hunger shows how, similar to the body’s requirement for nutrition from outside sources, people may need coaching to comprehend and successfully realize their inner desires. Without the right direction, they could make detrimental decisions repeatedly, just like when they consume “junk” without understanding their genuine needs. Mentorship serves as a compass, assisting people in discovering their true desires and fostering both personal and professional development. Think about your body, your purest form of
Navigating Chiropractic Frontiers
In this enlightening conversation, we dive deep into Dr. Lona Cook’s chiropractic journey, a chiropractor, coach, author, and visionary leader. Dr. Cook’s impact on chiropractic, her patients, her family, and the world at large is nothing short of inspirational. We listen to her as she shares her experiences from her chiropractic school days to building and scaling successful practices. Additionally, we explore her unique school program, coaching endeavors, and her profound insights on the intersection of chiropractic philosophy, energy awareness, and leadership. Chiropractic Odyssey: From School to Scaling Practices Dr. Cook’s journey began in chiropractic school at Northwestern, an institution with a strong medical orientation. Despite the initial lack of deep philosophical immersion, Dr. Cook’s trajectory took a transformative turn when she attended a New Beginnings seminar. Inspired by Dr. Eddie Diaz’s visualization exercise, she envisioned a world where everyone recognizes the vital role of chiropractic in a child’s health journey. This moment planted the seeds for her future endeavors. Scaling Practices: Fast-forwarding through her successful practice, Dr. Cook emphasized the importance of adapting and pivoting in response to unexpected challenges. While her initial dream was to establish one exceptional practice, she found herself opening a second practice due to personal circumstances. The partnership model, which involved mentoring and a structured buyout, allowed her to scale her practices successfully. Dr. Cook’s insightful perspective on partnerships highlights the significance of alignment, mutual respect, and shared goals for a thriving practice. Philosophical Foundations and Leadership: Dr. Cook delves into the philosophical foundations of chiropractic and the profound impact it has on her leadership philosophy. She emphasizes the importance of understanding metaphysics, epistemology, ethics, politics, and aesthetics—pillars that shape a chiropractor’s worldview. This philosophical depth informs her coaching approach, where leadership transcends mere management. Dr. Cook advocates for cultivating leaders who empower others, creating a ripple effect that extends beyond the chiropractic profession. School Program: Nurturing the Future One of the most captivating aspects of Dr. Cook’s journey is her pioneering school program, bringing chiropractic care to students. Inspired by a New Beginnings seminar, she initiated a program where chiropractors visit schools, initially for teachers and later for students. The program has expanded to multiple schools, with plans to replicate its success in other districts. Dr. Cook envisions a future where chiropractic care becomes an integral part of children’s health and well-being. Energy Awareness and Intuition: Dr. Cook shares her insights on energy awareness, intuition, and their profound impact on decision-making. Drawing from chiropractic philosophy and universal laws, she underscores the importance of recognizing vibrational frequencies in oneself and others. Dr. Cook’s approach aligns with the principle of strengthening strengths and outsourcing weaknesses, fostering a harmonious and impactful leadership style. Coaching with Dr. Cook: Dr. Cook offers coaching services tailored to chiropractors at different stages of their journeys. Prospective clients can initiate the process with a strategy call, where Dr. Cook gains insights into their aspirations and dreams. Her coaching spans from launching and building practices to supporting women in chiropractic who are navigating the complexities of leadership while juggling various roles. Conclusion: Dr. Lona Cook’s chiropractic odyssey is a testament to transformative leadership, aligning philosophy with action, and the profound impact of chiropractic care on individuals and communities. Her visionary initiatives, from scaling practices to pioneering school programs, reflect a commitment to empowering others and leaving a lasting legacy. As we conclude this conversation, Dr. Cook’s words resonate—a reminder that chiropractic is not just a profession; it’s a journey of self-discovery, leadership, and making a difference in the world. View the entire episode by accessing it through: https://bit.ly/3TX5IW7
Optimizing Chiropractic Teams
Today, we’re diving deep into the world of chiropractic hiring with Dr. Mark Mouw, the founder of Chiro Match Makers. Dr. Mouw, a successful clinic owner and coach of The Remarkable Practice, is here to share insights on the challenges of finding the right chiropractic associates and how Chiro Match Makers is transforming the hiring process. Finding the Right Fit: Dr. Mouw kicks off the discussion by emphasizing the critical importance of hiring the right person for the right role to ensure success. With Chiro Match Makers, they have honed in on a strategic approach, utilizing behavioral assessments to identify the best match for chiropractic practices. This is not just about finding any associate but discovering the right fit to achieve long-term synergy. The Evolution of Chiro Match Makers: Dr. Mouw takes us on a journey through the inception of Chiro Match Makers, highlighting the collaborative effort of Dr. Steven France, Dr. Ellen Miner, Sheila, and himself within The Remarkable Practice. Initially focusing on hiring chiropractic assistants (CAs), they soon expanded to include associate searches, addressing a significant need in the profession. Understanding Chiropractic Personalities: The conversation delves into the three main types of chiropractors identified through behavioral assessments: entrepreneurs, business builders, and caregivers. Dr. Mouw breaks down their traits and percentages within the profession. Notably, caregivers make up the majority (65%), seeking fulfilling patient relationships without the desire to run a business. Overcoming Hiring Pitfalls: Dr. Mouw addresses common hiring mistakes, emphasizing the tendency of chiropractors to hire individuals similar to themselves. This leads to challenges when hiring entrepreneurs or business builders who may eventually seek to open their practices, resulting in turnover. Chiro Match Makers aims to shift this paradigm by creating a language of understanding and aligning individuals with complementary traits. The Power of Behavioral Assessments: The Chiro Match Makers team uses licensed behavioral assessments that are EEOC compliant, providing valuable insights into an individual’s behavioral traits. By understanding these traits, practices can strategically build a team that complements each other, fostering a collaborative and successful environment. Scalability and Vision: Dr. Mouw emphasizes the importance of having a clear vision for the practice and building a team that aligns with that vision. The scalability of a practice relies on training, accountability, and autonomy for team members. This approach enables chiropractors to step back from daily operations, promoting long-term stability and durability. Legacy and Exit Strategies: The conversation concludes with insights into legacy-building and exit strategies. Dr. Mouw discusses the four main reasons chiropractors seek assistance: time freedom, increased revenue, stability and durability, and legacy building. Chiro Match Makers and The Remarkable Practice offer comprehensive support, whether it’s finding the right associates or navigating the process of selling a practice. Conclusion: In the dynamic world of chiropractic hiring, Chiro Match Makers and Dr. Mark Mouw stand as beacons of innovation. By incorporating behavioral assessments and strategic insights, they are revolutionizing the way chiropractors build teams and shape the future of their practices. As the profession evolves, finding the right fit becomes not just a necessity but a transformative journey towards success. To watch the full episode, you may view it via: https://bit.ly/48AU07C
Building Empires of Health
In the ever-evolving landscape of healthcare, few stories are as compelling as that of Dr. Jeff Danielson, a chiropractor, visionary entrepreneur, and the mastermind behind Big Fish Enterprises. In an exclusive podcast episode, Dr. Danielson shares the intricate details of his journey, offering listeners a glimpse into the unique blend of chiropractic expertise and business acumen that has propelled him to success. The Genesis of a Visionary: Dr. Jeff Danielson’s story begins in Minneapolis, Minnesota, where he not only thrived as a chiropractor but also cultivated a keen entrepreneurial spirit. It was during his interactions with students at a chiropractic school that he recognized a recurring pattern: young, talented chiropractors eager to make a difference, but often left unsupported after a brief stint in his practice. This realization led to the birth of an innovative coaching program. “Pay It Forward” Philosophy: The heart of Dr. Danielson’s coaching philosophy lies in the concept of “Pay It Forward.” He sought to break the cycle of talented chiropractors leaving after gaining experience and knowledge. Instead, he envisioned a system where associates would be mentored, trained, and ultimately become partners in the journey of acquiring and transforming chiropractic practices. This unique approach has not only benefited Dr. Danielson’s clinics but has created a ripple effect of success through the chiropractic community. Big Fish Training: Transforming Practices: The coaching program, aptly named Big Fish Training, was designed to turn ordinary practices into thriving enterprises. Dr. Danielson emphasizes a hands-on approach, pairing associates with him in his own practice, imparting not just clinical knowledge but the critical skills needed to run a successful chiropractic business. The goal is to transform practices from mere “Ford Taurus” models to high-performance “Lexus” clinics. Team Doc: Revolutionizing Community Engagement: One of Dr. Danielson’s game-changing innovations is Team Doc, a program that redefines community engagement and patient acquisition. By sponsoring local sports teams, especially those in unexpected niches like trap shooting, Dr. Danielson creates opportunities for meaningful connections. This unconventional marketing strategy has proven wildly successful, with dozens of new patients generated from each event, further solidifying the impact of chiropractic care in the community. Chiro Life: A Platform for Transformation: Dr. Jeff Danielson’s commitment to sharing knowledge and fostering collaboration reaches its zenith with the Chiro Life seminar. This annual event is a testament to his vision of building a community of chiropractors who not only excel in their practices but also inspire and support one another. The upcoming seminar, themed “Build Your Army,” promises to be a transformative experience, featuring speakers like Brian Capra, Jeff Langmaid, and Roberto Monaco. Conclusion: Dr. Jeff Danielson’s podcast episode is a masterclass in combining passion, purpose, and business savvy to create a lasting impact in the chiropractic world. His journey, from a chiropractic clinician to a mentor shaping the future of the profession, is an inspiration to aspiring chiropractors and entrepreneurs alike. As the chiropractic community eagerly anticipates the Cairo Life seminar, Dr. Danielson continues to shape the narrative of success in chiropractic care and business. To watch the full episode, you may view it via: https://bit.ly/3TK2qoS
Value Adding for Maximum Profit
I love this topic because it’s easy to miss the mark, especially since so many consultants and marketing firms misappropriate this term and don’t actually coach on value-adding. The idea of value-adding has come under scrutiny in light of the current trend of corporate acquisitions of primary care clinics and the rising patient expectation for comprehensive, patient-centered treatment (Abelson, 2023). This is because of how the healthcare industry is changing. There is a growing need to separate actual value addition from empty rhetoric when corporate companies acquire primary care operations. The demand for genuine, efficient value-adding solutions has never been greater due to the rise in patient expectations for a comprehensive healthcare experience. Don’t get me wrong, plenty do an absolutely amazing job, and their clients see great results, but more often than not, disaster strikes. Especially in the case of Joseph and Bonnie… When Joseph and Bonnie opened their practice, they were die-hard, convinced that they only needed to practice their specialty and nothing else. If we stay true to our specialty’s expertise and principles, we shouldn’t need anything else in the practice to thrive. Although reasonable, this viewpoint failed to consider the changing expectations of healthcare consumers. Patients are increasingly looking for holistic healthcare that covers their current requirements and their long-term well-being, according to Yussof et al. (2022). This suggests Joseph and Bonnie’s single-focused strategy didn’t meet the patient’s desire for comprehensive care. Today’s patients want treatments that address their current health needs and promote wellness, including preventative and long-term health management. Thus, healthcare professionals who offer more services are valued more. So they went about building out a space with the money their mentor had given them and whatever they could find and were adamant that physical therapy was the only service to be offered. Once the space was open, they began marketing to orthopedists in the area and getting patient referrals. That’s when the opportunities opened up. Patients started asking about ancillary services they didn’t have, making them feel like they looked silly. Patients asked about home fitness programs, nutrition, supplementation, and other specialties like Chiropractic or group fitness. The study by Patel & Singhal (2023) demonstrates the growing tendency of patients to seek comprehensive care. It showed that most patients favor healthcare facilities that offer various services under one roof. Patients increasingly view healthcare as a holistic activity. They want nutrition advice, exercise regimens, and alternative cures, not just specialist therapy. This shift in patient preferences fuels the desire for multi-service healthcare facilities that can meet several health and wellness goals. Initially, Joseph and Bonnie ignored it and kept progressing, growing at around 10%. They did a first-quarter review, and it was clear they were not on track to meet their financial freedom goals. They were convinced that something had to change, but they knew working harder to build new referring relationships was not scalable. They could only see so many patients daily, and hiring more therapists would add to their overhead. They needed a solution that minimized overhead growth while maximizing potential revenue. Joseph and Bonnie started taking patient requests seriously and realized a clear pattern. Patients were looking for wellness, not just treatment. Patients wanted to know if they could have a one-stop shop for preventative and therapeutic care. This was a new concept to Joseph and Bonnie, but they began exploring it and found an incredible and vast potential revenue stream in things like product offerings, DME, and more. Such a change toward integrated healthcare delivery is consistent with the ongoing tendency within the pharmaceutical sector to develop into wellness providers with patient-centric services (Moreno, 2019). This represents a larger healthcare shift from treating sickness to promoting well-being. Pharmaceutical corporations are expanding their position to include disease prevention, wellness, and patient-centric services for different health needs. Patients want a single source of preventative and therapeutic care. At first, Joseph and Bonnie only wanted to add what they could manage and keep the specialty singular. However, it soon became clear that their patients were looking for a more sophisticated preventative care so they hired a part-time nutritionist who turned into a full-time nutritionist. They bought used fitness equipment and hired a part-time fitness instructor who turned into a full-time instructor (Joseph recently replaced this person as the full-time trainer because of his personal love of fitness; the perks of being the boss). So what is value adding? Is it simply the addition of multiple complementary specialties into your practice? Maybe. Recent developments in primary and pharmacy care have demonstrated that value addition can be achieved by implementing cutting-edge health methods like digital medicines and remote patient monitoring (Smith, 2021). Value-adding extends beyond incorporating diverse specialties. Digital medicines and remote patient monitoring improve patient care and convenience. These strategies satisfy patients’ desire for individualized, accessible treatment, bringing value to a practice. It could also be the addition of community events, marble floors in the patient bathroom, or a cooling station with fancy refreshments. The true value add in a practice is unique to the patient community. It’s a matter of listening to the value-adds they seek and finding a way to accommodate them that supports the larger purpose and mission. If your practice is in a really nice part of town and you managed to get a great deal on space but are short on cash, it could be a matter of setting up one fancy area in your practice that you can afford to spruce up (it should also be functional, before you go replacing drapes). Whatever change you attempt needs to address two things: Patient requests – Surveys often help the most in this area Patient function – You want the value to add(s) to be usable in some way that improves the patient’s experience both individually and as a group A fancy cooling station with multiple settings, fruit, vegetable-enhanced water, and more can get patients talking and feeling fancy. Often these changes can also help enhance the practice’s
Maximizing Chiropractic Efficiency: The Power of Integrated Software Solutions
In today’s digital age, the healthcare industry, including chiropractic practices, is rapidly evolving. With the rise of technology, there’s an increasing need for integrated software solutions that can streamline operations, enhance patient experience, and boost overall efficiency. In this context, the integration of platforms like Genesis Chiropractic Software and TrackStat is nothing short of revolutionary. The Need for Automation in Chiropractic Practices Automation is no longer a luxury but a necessity. With the increasing demands on healthcare professionals, manual processes can become tedious and prone to errors. By automating tasks such as patient management, appointment scheduling, and follow-ups, chiropractors can ensure a smoother and more efficient workflow. This not only saves time but also reduces the chances of human error, ensuring that patients receive consistent and high-quality care. Segmentation for Personalized Patient Care One size doesn’t fit all, especially in healthcare. Every patient is unique, with different needs and health conditions. By segmenting patients into different categories based on their health conditions, treatment plans, or other criteria, chiropractors can offer more personalized care. This not only enhances the patient experience but also ensures that each patient receives the most appropriate and effective treatment. The Power of Sales Pipelines in Patient Conversion A robust sales pipeline is crucial for any business, including chiropractic practices. By tracking new patients, their last and next visits, and other relevant information, chiropractors can gain valuable insights into their conversion rates. This data can be instrumental in identifying areas of improvement and implementing strategies to boost patient conversion. Enhancing Patient Retention with Data Analytics Patient retention is a critical metric for any healthcare practice. By analyzing data on patient drop-offs, chiropractors can identify specific points in the patient journey where they’re losing patients. With this information in hand, they can implement targeted strategies, such as educational workshops or progress exams, to enhance patient retention. Streamlining Operations with Two-Way Texting and Smart Reactivations Communication is key in healthcare. Two-way texting allows for seamless communication between chiropractors and their patients, ensuring that patients are always informed and engaged. Additionally, smart reactivations can help chiropractors identify and reach out to patients who haven’t been in for a while, ensuring that they continue to receive the care they need. Reducing Accounts Receivable with Integrated Solutions Financial health is crucial for the sustainability of any practice. By integrating solutions that help reduce accounts receivable, chiropractors can ensure a steady cash flow and financial stability. This not only ensures the smooth running of the practice but also allows chiropractors to invest in further enhancing their services. Conclusion The integration of platforms like Genesis Chiropractic Software and TrackStat offers a plethora of benefits for chiropractic practices. From automating tasks to enhancing patient experience and boosting efficiency, these integrated solutions are truly game-changers. As the healthcare industry continues to evolve, it’s crucial for chiropractors to leverage the power of technology to stay ahead of the curve and offer the best possible care to their patients. Note: For a deeper dive into these topics and to hear firsthand experiences from industry experts, watch the video at the top of this page.
Why ClinicMind?
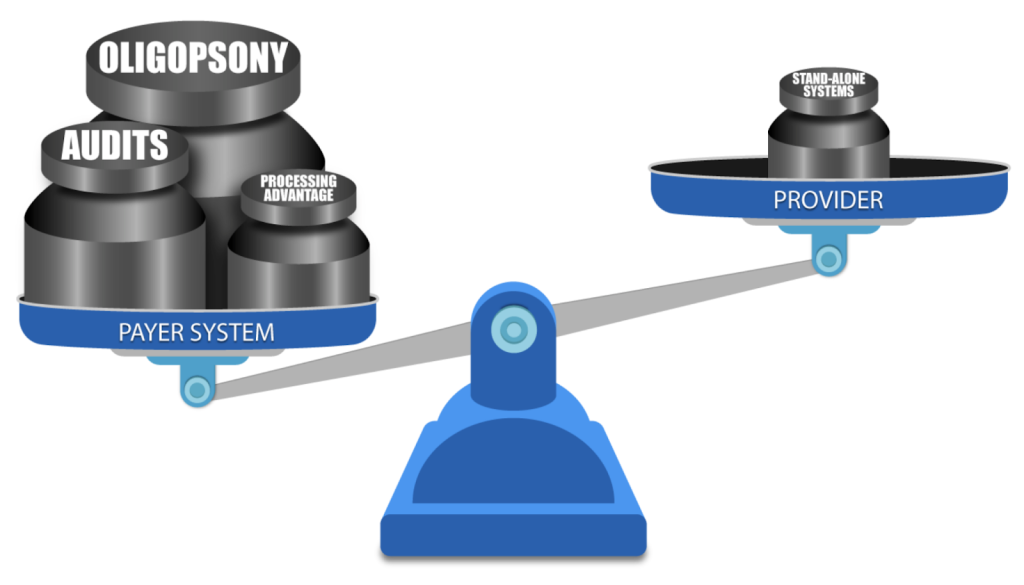
DO YOU know a practice owner who wants more patients in her clinic, better pay-per-visit, and better collections? We all know healthcare practice owners who want to remain independent and grow and yet are frustrated by insurance companies and continuous battles to get paid and stay compliant. Now, as a patient, do you like visiting a healthcare practice, receiving bills, and reconciling them with your insurance company? You are not alone. As it turns out, most other people do not like their patient experience. The problem is that patient and independent practice needs have evolved in step with society and technology, but management methodology remained in the 19th century. There’s a fundamental mismatch between how healthcare practices and patients are managed — and the practice owners’ and patients’ expectations. We came to a startling observation: patients no longer want their care to be managed the way it used to be managed in the previous century. And yet, practice owners still use their old methods to memory-manage their practice. Who is taking advantage of this mismatch? The insurance companies – payers. From the outset, we knew that healthcare costs are spiraling out of control. We also knew that insurance companies, medical equipment manufacturers, pharmaceuticals, and hospital executives have been all making handsome returns and benefitting from healthcare cost growth. One question bothered us: why are the practice owners unable to participate in that growth? How was it that the key contributors to healthcare service were excluded from fair compensation for their work and grew exceedingly frustrated with rules and regulations? Some providers were selling their practices to join larger networks or hospitals, and others were moving to different industries. National studies have shown that physician burnout rates are climbing up. For instance, Mayo Clinic Proceedings reported that the prevalence of burnout among U.S. physicians was 63% in 2021, compared with 38% in 2020, 44% in 2017, 54% in 2014, and 46% in 2011. We also noticed that with experience, medical billing managers start cherry-picking insurance companies for easy follow-up. So, the practice owners could not get paid on time and in full by a growing number of insurance companies (payers). The more obstacles payers pose – the less paid the providers are. Payers were stacking the game against the providers by continuously adding new rules to reduce payments and increasing the frequency of provider audits. In addition to continuous consolidation, resulting in scarcity of payers (a market structure known in economics as Oligopsony), which allows the payers to drive the reimbursement fees down, they also have a two-pronged resource advantage: attract Ivy-league MBAs to build sophisticated claim-processing protocols and discover every little pretext to deny or delay claim payment leverage the most powerful digital technology to implement those protocols on the ever-growing volume of claims. ClinicMind was founded to address two basic challenges facing providers: a patient-provider expectations mismatch and payer-provider adversity. First, the patients have transformed how they expect healthcare service delivery, but practice owners have not adapted their practice management methodology. Second, insurance payers underpay and delay payments because they make a substantial profit from the “float.” The float is the money insurers hold onto between the time they collect premiums and the time they pay out claims. In summary, 1. The Basic Mismatch Between Patients and Providers: a. Background: The healthcare industry has undergone significant changes in recent years, with patients becoming more proactive in managing their healthcare and demanding a different level of service. This transformation is largely due to increased access to health information through the Internet and the rise of patient-centered care models. However, many practice owners, particularly in traditional healthcare settings, have not adapted their practice management methodology to meet these changing patient expectations. b. Conflict: Patient Expectations: Patients today expect convenience, transparency, and a more personalized approach to healthcare. They want to schedule appointments online, access their medical records easily, and receive timely, clear communication from their healthcare providers. Provider Resistance: Many practice owners and healthcare providers are accustomed to traditional, paper-based methods and may hesitate to embrace digital technologies or change their established processes. This resistance can result from the comfort with the status quo, fear of the unknown, or high implementation costs. c. Resolution: To resolve this conflict, healthcare practices must adapt to the changing landscape. This may involve investing in electronic health records (EHR) systems, online appointment scheduling, telemedicine services, and more. Additionally, training staff and providers to use these technologies effectively is crucial. Clear communication with patients about these changes, the benefits they bring, and how data security and privacy are maintained can help build trust and reduce resistance. 2. Payer-Provider Adversity: a. Background: In the healthcare system, insurance payers (such as health insurance companies) often maintain a substantial portion of their profit through a financial mechanism called the “float.” The float is the money insurers hold onto between the time they collect premiums and the time they pay out claims. This float can represent a significant source of income for payers. However, it can create a conflict of interest with healthcare providers. b. Conflict: Payer Profit: Insurance payers benefit from maintaining a healthy float, as they can invest these funds and earn returns. The larger the float, the more profit they can potentially make. Payers have a significant advantage over the providers because of the oligopsony and because of significantly larger resources for better talent hiring and data processing. Provider Concerns: Healthcare providers, on the other hand, often face challenges in receiving timely and appropriate payments from payers. Delays or disputes in claims processing can impact their cash flow and ability to provide care. Providers feel that payers prioritize maintaining their float over ensuring prompt reimbursement. c. Resolution: Transparency and fair contracting: Establish clear and fair contracts between payers and providers that outline payment terms, including prompt payment schedules and dispute resolution mechanisms. Industry consolidation: Metcalf’s Law states that the value of a network is

