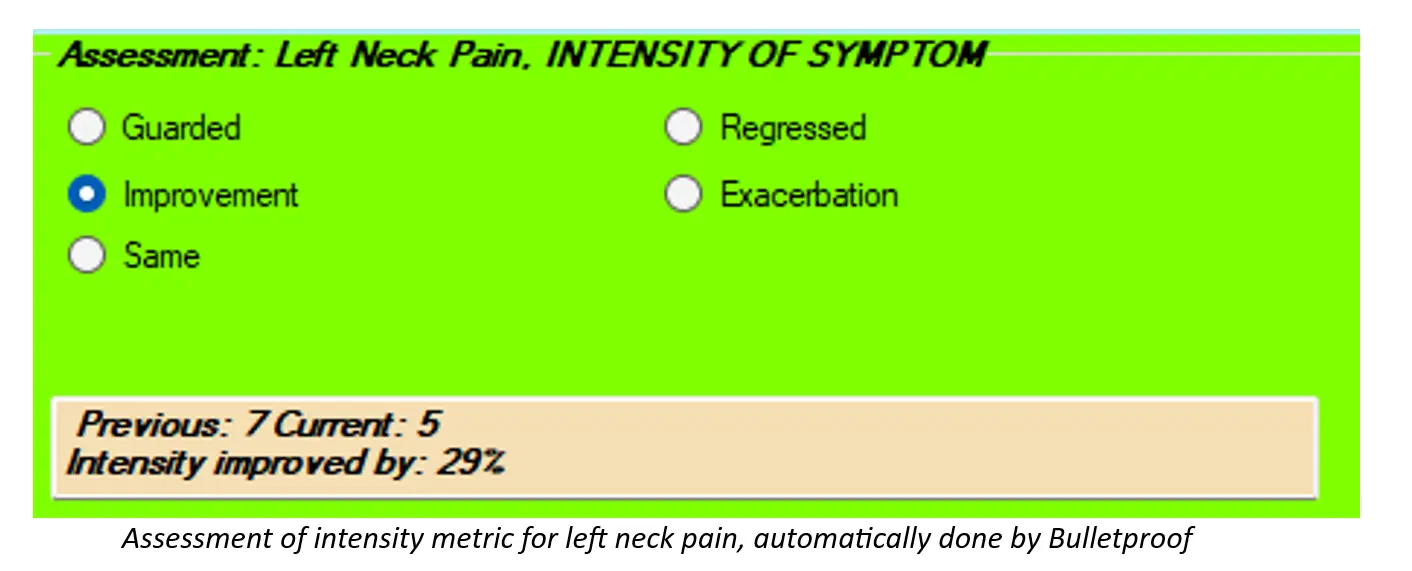
There’s ONE part of our SOAP notes that I’ve been preaching about for years, but it seems as though not many doctors are paying close enough attention to it. It’s the Assessment. Here’s what I see in most records that I review in the Assessment part of the SOAP Note: “Patient is responding well to care.” “Patient is the same.” “Patient is responding slower than expected.” To begin with, according to our friends at Centers for Medicare and Medicaid Services (CMS), we are to document an assessment for each condition that we are treating. If we’re treating a patient for headaches, neck pain and upper back pain, we need to document an assessment for each of these. Even though I’m talking about Medicare, and you may see very few Medicare patients, just remember that Medicare creates the rules that most insurers (and even state boards) follow. If we document well for Medicare, we’re that much closer to the promised land. OK, back to my point. The next thing that Medicare is looking for in the Assessment is how each condition is on today’s visit as compared to the previous visit. That can be problematic. Do they really expect us to look back a visit every time the patient comes in and we have to compare that visit to today’s visit? And what if, on the previous visit, we said something like “Patient presents with neck pain” and on today’s visit we write, “Patient presents with neck pain.” See the problem? Then Medicare wants us to document the effectiveness of our treatment for each condition as compared to the previous visit. Seriously? If you’ve been reading my previous blog posts, you’ll remember that I’m making a big deal about us using certain metrics with our documentation. By using these metrics, we can actually document how each condition is responding since the previous visit AND the effectiveness of our treatment. That’s easy with the right technology. I recently looked at notes from an Administrative Law Judge in a Medicare audit. The particular doctor being audited did a pretty good job of documenting P.A.R.T. and most likely thought he was in the clear. Not so much. The judge noted, for all claims audited, that the doctor failed to document how each condition had changed since the previous visit AND the effectiveness of treatment. Medicare wants their money back – the tune of TENS of THOUSANDS of DOLLARS. If there are any complicating factors, specific to each condition, that may slow the patient’s recovery for that condition, we can document those, too. I make sure that these complicating factors appear on every visit in my SOAP notes. Finally, we can document the diagnoses under Assessment. It really doesn’t matter where in your soap notes you put the diagnoses, but Assessment seems to be the most logical. You’ll want to document both the ICD10 code AND the description, though, not one or the other. Instead of thinking about the Assessment as a pain in the ASSessment, we can think differently about it so we can use it in our favor – by showing the world how awesome chiropractic is and how effective our treatment is – both quantifiably and functionally.
Gregg Friedman, DC, CCSP, FIACA
Creator of The Bulletproof Chiro EMR