Let’s Have More Fun-ction

More about… Medicare, Medicare, Medicare. In my last article, I wrote about the TWO THINGS that Medicare wants from us. The first thing is PAIN. So now, let’s discuss the SECOND thing Medicare wants from us. Function Medicare requires that we perform a Functional Outcome Assessment for our patients. They define a Functional Outcome Assessment as “patient completed questionnaires designed to measure a patient’s limitations in performing the usual human tasks of living and to directly quantify functional and behavioral symptoms.” But… They also state that we must use a “standardized tool” and document a care plan “based on the identified functional outcome deficiencies.” And… They continue…“Documentation of a current functional outcome assessment must include identification of the standardized tool used.” So what is a “standardized tool?” According to Medicare, it’s “a tool that has been normalized and validated.” That means you can’t just make one up. But there’s more… Medicare also states that “A functional outcome assessment is multi-dimensional and quantifies pain and neuromusculoskeletal capacity; therefore the use of a standardized tool assessing pain alone, such as the visual analog scale (VAS), does not meet the criteria of a functional outcome assessment standardized tool.” So how often do we need to have our patients do these? Medicare states, “The intent of this measure is for a functional outcome assessment tool to be utilized at a minimum of every 30 days.” But there’s more… Here’s Medicare’s rationale: “Standardized outcome assessments, questionnaires or tools are a vital part of evidence-based practice. Despite the recognition of the importance of outcomes assessments, questionnaires and tools, recent evidence suggests their use in clinical practice is limited. Selecting the most appropriate outcomes assessment, questionnaire or tool enhances clinical practice by (1) identifying and quantifying body function and structure limitations; (2) formulating the evaluation, diagnosis, and prognosis; (3) informing the plan of care; and (4) helping to evaluate the success of physical therapy interventions (Potter et al., 2011).” Medicare also tells us that “clinicians should use validated self-report questionnaires/tools that are useful for identifying a patient’s baseline status relative to pain, function, and disability and for monitoring a change in a patient’s status throughout the course of treatment.” Remember what I told you in my last article, though. Medicare drives this whole train. Everyone else follows Medicare. They created the documentation guidelines. They guide the CPT and ICD10 codes. So, instead of fighting them (and losing), we need to understand their perspective and follow their rules. So, let’s break this down. For ALL of our patients, regardless if they’re a Medicare patient, cash-paying patient, personal injury patient or anyone else – it’s time we standardize this ONE thing – our documentation. Document the pain intensity and pain frequency for each complaint on every visit. Have the patients complete a functional outcome assessment utilizing a standardized tool. Document the name of each functional outcome questionnaire and its score. Formulate a treatment plan based on the functional outcome assessment score. And don’t panic. This can be done in very little time. The results are worth it. Be BulletProof.
What a Pain

Medicare, Medicare, Medicare. I know, we’ve had this hate-hate relationship with them for so many years. So many chiropractors are afraid of it and hate the reimbursement. I get it. But… You need to understand that Medicare drives this whole train. Everyone else follows Medicare. They created the documentation guidelines. They guide the CPT and ICD10 codes. So, instead of fighting them (and losing), how ‘bout we understand their perspective a bit more. Medicare wants TWO things from us. The first thing is PAIN. In 2009, the American Pain Foundation identified the following pertinent facts related to the impact of pain: 76.5 million Americans suffering from pain. Pain affects more Americans than diabetes, heart disease and cancer combined. It is the number one reason people seek medical care. Uncontrolled pain is a leading cause of disability and diminishes quality of life for patient, survivors, and their loved ones. It interferes with all aspects of daily activity, including sleep, work, social and sexual relations. Under-treated pain drives up costs – estimated at $100 billion annually in healthcare expenses, lost income, and lost productivity – extending length of hospital stays, as well as increasing emergency room trips and unplanned clinic visits. Medically underserved populations endure a disproportionate pain burden in all health care settings. Disparities exist among racial and ethnic minorities in pain perception, assessment, and treatment for all types of pain, whether chronic or acute. Stewart et al. (2003) identified almost thirteen percent of the total workforce experienced a loss in productive time during a two-week period due to a common pain condition: 5.4% for headache; 3.2% for back pain; 2.0% for arthritis pain; 2.0% for other musculoskeletal pain. What does Medicare want from us with regard to documenting PAIN? They simply want us to document a pain assessment using a standardized tool(s) on each visit AND documentation of a follow-up plan when pain is present. There are a number of standardized tools that Medicare gives as examples, but the easiest and fastest is the Verbal Numeric Rating Scale. This is the familiar 0-10 scale, with 10 being the worst pain imaginable. Add to that the % of time the patient notices that condition, and you’ve got Pain Assessment locked up. Be BulletProof.
The What and The Why
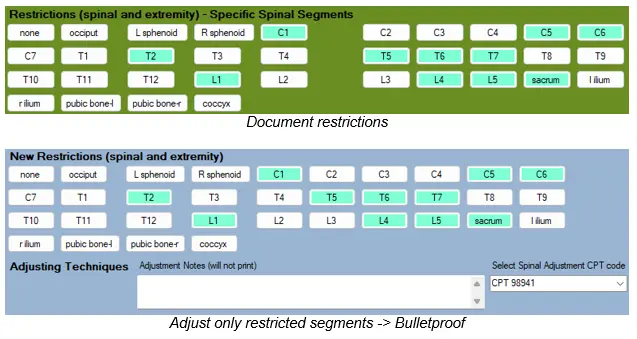
When we think of documenting a SOAP note, we need to be sure that we connect all the dots. One of the biggest problems I see in the many chiropractic records I review is that the treatment is not justified by the findings. And it’s easily corrected. If you perform an adjustment/CMT at C3, what is the justification for that? The simple answer is restriction/fixation/subluxation at C3. If you perform an adjustment/CMT to the right shoulder, the justification would be restriction/fixation/subluxation of the right shoulder. You also want to be sure there is asymptomatic complaint and diagnosis that corresponds to the finding. Think of it this way: symptom + finding + diagnosis = justification for treatment. Manual Therapy (97140) Manual Therapy is another one that comes up frequently. CPT tells us that manual therapy (97140) is performed in order to increase functional performance, increase range of motion, decrease inflammation and reduce muscle spasm. That tells us that our objective findings should mention some type of decrease in functional performance, decrease in range of motion, increase in inflammation or the presence of muscle spasms. Therapeutic Exercise (97110) CPT tells us that therapeutic exercises are performed in order to develop strength and endurance, range of motion and flexibility. The justification that we should document for this should mention some type of abnormality of strength and endurance, range of motion or flexibility. When we document properly and understand that the Why supports the What, we’re one step closer to being… BulletProof.
How to Document for Wellness Patients

This question comes up periodically. “What do we need to document for our maintenance patients?” Let’s first define what we mean by “maintenance” patients. Some of these patients come in with no symptoms – they just like to get adjusted periodically. Other patients, though, have some level of chronic pain or discomfort that never seems to go anywhere – it just stays the same all the time and they find that getting chiropractic care keeps it from getting worse. The type of care these patients get is called “supportive care.” For the asymptomatic maintenance patients, we still need to document a SOAP note for them. Here’s what I recommend: 1. For Subjective Complaints, you can simply document “Patient X is here today with no symptoms, for the purpose of a maintenance adjustment.” 2. For Objective Findings, if you plan on adjusting them, document the restrictions/subluxations, but at specific levels, like C3, T4 and so on. If there are any muscle spasms or trigger points, make sure you document them. 3. For Assessment, there are no metrics to consider, so there’s no need to compare to the prior visit. However, you should still document the diagnoses, both code and description. 4. For Plan, document what you did. If you adjusted the patient, make sure you document the specific segments adjusted. For patients receiving “supportive care,” you should still document the metrics of pain intensity and pain frequency, even if they don’t change much. Document your daily findings (Asymmetry/Misalignment, Range of Motion Abnormality, Tissue/Tone Changes). If you are adjusting the patient, definitely document the spinal/extremity restrictions (asymmetry/misalignment). If you perform any other treatment, make sure each procedure is properly justified in your SOAP notes. Document the Assessment, which should include complicating factors and diagnoses. Does anyone actually PAY for supportive care anymore? Every now and then, but not too often. Workers Comp has paid for supportive care in the past, but they’re starting to move away from it. This is something the patients should pay for out of their own pocket. Be BulletProof.

