After being in practice for 32 years, teaching documentation and coding for about 20 years, reviewing records and performing IMEs for a lot of years, I see and hear the same things over and over again with regards to documenting subjective complaints. Let’s make this easy.
Initial Visit
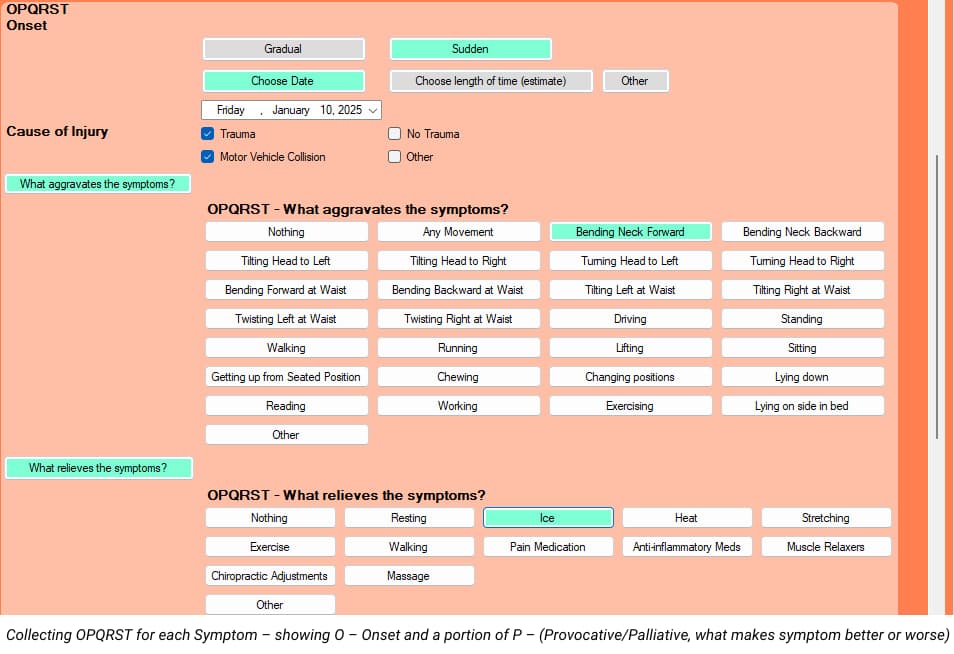
According to the Mayo Clinic, 80% of the proper diagnosis comes from a good history. Unfortunately, many chiropractors tend to take shortcuts on the history, perhaps in the interest of saving time. The standard of history taking has been the OPQRST for many years. There are a few variations of this, but they all tend to get the same information. Before you think of not asking and documenting all of OPQRST, think about which of these items are less important than others. I teach doctors to document ALL of OPQRST on the first visit for ALL new patients, but there’s an easy and fast way to do it. Once we get that information at the beginning of a case, we don’t have to document all of that on subsequent visits. So, let’s review the OPQRST:
Onset – when the patient presents with multiple conditions for which you will treat, you need to document OPQRST for EACH complaint, not just the CHIEF complaint. You’ll want to document how each condition started (trauma vs. no trauma), when each condition started (specific date or time frame) and if each symptom began suddenly or gradually.
Provocative/Palliative – document both provocative and palliative for EACH condition you’ll be treating. In other words, what makes the neck pain better and worse, what makes the low back pain better and worse, etc.
Quality – describe the quality of EACH symptom you’ll be treating.
Radiate – document if each condition is radicular or not. If a symptom is radicular, use the language of Anatomical Position so anyone seeing your records will know what you’re talking about. For example, in the language of Anatomical Position, “arm” refers to above the elbow and “forearm” refers to below the elbow. “Thigh” refers to above the knee and “leg” refers to below the knee. You can be specific by documenting the neck pain radiates to the right posterolateral arm, right posterolateral forearm and to the first 2 digits of the right hand.
Site/Severity – Be specific without going overboard. Instead of documenting “headaches”, we can document “occipital headaches.” For neck and back pain, we can document if it’s the whole neck or back or left or right. For severity, more and more payers and even reviewers like me want to see a 0-10 pain scale (10 being the worst pain imaginable) for each complaint. To make this easier for my patients, I start by asking them if they would call their pain, for each symptom, Mild, Moderate or Severe. If they say Mild, I explain that’s between a 1 and a 3 and ask them for a number. For Moderate, that’s between a 4 and a 7, and for severe, that’s between an 8 and a 10. That tends to make it easier for them to come up with a more accurate number. So, ask verbally for mild, moderate or severe for each symptom, but only to get them to an actual number that you’ll document.
Timing – On the first visit only, document, for each symptom that you’re treating, if the pain is worse at a particular time or times of the day (morning, afternoon, evening, night), or if the symptom is unaffected by time of day. For all visits, document what percentage of their awake time they notice each symptom. BEWARE of using the ranges of Occasional, Intermittent, Frequent and Constant, though. These ranges are defined as:
Occasional: 0-25% of awake time
Intermittent: 26-50% of awake time
Frequent: 51-75% of awake time
Constant: 76-100% of awake time
The problem with these ranges is that they’re too broad (25 points). Your patient’s symptom could appear stuck in a particular category for MONTHS, which can make your documentation weaker by showing no change. Instead, I recommend document an actual percentage of time that each symptom is noticed (5 or 10 percent increments, though-don’t get carried away by documenting “23% of the time.” If you document on one visit that the frequency of the symptom was 100%, but on the next visit it reduced to 95%, even though just a slight change, it’s still shows some improvement. It’s much better to show the frequency went from 100% to 95% to 90% to 85% to 80% to 75% than to show constant, constant, constant, etc.
Gregg’s Tip: I designed my intake paperwork to capture all of this information, so my patients do all of the heavy lifting for me. We send them the paperwork via e-mail and instruct them to bring the completed forms with them to their appointment. I also designed my EMR to be the same flow and direction of my paperwork, which makes it MUCH easier for the doctor or staff to input the information. Once we get all of that information entered on the first visit, all subsequent visits are QUICK AND EASY – I just change the metrics of the Severity and Frequency of each symptom.
The next part of documenting subjective complaints is to establish a “measurable baseline of function” for each complaint. A great, easy, fast and inexpensive way to do this is with valid and reliable outcome questionnaires. Medicare requires this, many commercial insurers require this and for workers comp and PI, us reviewers are looking for this. You want to document the scores on the outcome questionnaires on the very first visit, which can then be used as a treatment goal. While Medicare requires that we perform these functional outcome assessments at a MINIMUM of every 30 days, I recommend performing these outcome questionnaires every two weeks for the active patient and once or twice per year for maintenance patients. If all chiropractors would do these outcome questionnaires every 2 weeks for ALL active patients, our documentation would be tremendously improved overnight.
Gregg Friedman, DC, CCSP, FIACA
Creator of The Bulletproof Chiro EMR