Update on PatientHub Appointment Management Issue
Update – January 10, 2024 We’re pleased to inform you that the PatientHub Appointment Management Issue has been fully resolved, patients will continue to receive appointment reminders, and all systems are now back up. We sincerely appreciate your patience and understanding during this time. If you experience any issues or have any questions, please don’t hesitate to reach out to our support team. Update – January 9, 2024 We want to inform you about a technical issue affecting the PatientHub appointment management. Our development team is actively working to resolve it as quickly as possible. Here’s what you need to know: Appointment Reminders for Existing Bookings: Patients who booked appointments before today will still receive their reminders as usual. Impact on New Appointments: New appointments may be temporarily affected until the issue is resolved. While we cannot provide a specific timeline for the complete restoration of the service, we will share updates as progress is made. We sincerely apologize for any inconvenience this may cause and greatly appreciate your patience. If you have urgent concerns or need assistance, please don’t hesitate to contact our support team. Thank you for your understanding and trust.
Save Time and Improve Patient Care with the Encounter Bar
The Encounter Bar in the Chart Summary is designed to simplify access to patient visit history, reduce clicks, and improve workflow efficiency. Why the Encounter Bar Is a Game-Changer: Comprehensive Overview: View a patient’s full visit history, including past, current, and upcoming appointments, all in one place. Streamlined Navigation: Say goodbye to repetitive navigation and wasted time searching for key details. Access everything you need with fewer clicks. Improved Decision-Making: With all relevant visit information at your fingertips, providers can make informed decisions faster and improve patient care. Why It Matters: The Encounter Bar allows providers to focus on what truly matters: delivering high-quality care. By reducing workflow interruptions and simplifying navigation, this feature enables your team to save time, streamline operations, and improve patient outcomes. Interested in optimizing patient flow for your practice? New Clients: Book a consultation to learn how these features can transform your workflows. Current Clients: Reach out for a detailed training session and discover how to make the most of this feature for your practice.
Optimize Patient Flow and Eliminate Bottlenecks with the Rooming Module
We’re excited to highlight the Rooming Module, a game-changer in real-time patient flow management. Efficient patient movement is essential to ensure smooth visits, reduce wait times, and improve the overall care experience. How the Rooming Module Helps Your Practice: Real-Time Tracking: Know where patients are at every stage of their visit, enabling seamless transitions between rooms and reducing wait times. Eliminating Bottlenecks: Automate room assignments and transitions, allowing your staff to handle patient flows more effectively and minimize delays. Enhanced Communication: With instant updates on patient location, your staff and providers can collaborate better and deliver timely care. Workflow Efficiency: From check-in to rooming, every step is accounted for, simplifying daily operations for your team. Why It Matters: Whether your practice manages single appointments or complex schedules, the Rooming Module optimizes workflows to ensure your patients receive the care they need without unnecessary delays. Interested in optimizing patient flow for your practice? New Clients: Book a consultation to learn how these features can transform your workflows. Current Clients: Reach out for a detailed training session and discover how to make the most of this feature for your practice.
The Rise of Telehealth: Revolutionizing Healthcare for a Digital Age

The healthcare landscape has undergone significant transformations in recent years, with Telehealth standing out as one of the most impactful innovations. What was once seen as a niche service is now a mainstream solution, enabling healthcare providers to reach patients no matter where they are. As technology continues to evolve, Telehealth is shaping the future of healthcare, improving access, efficiency, and the overall patient experience. What is Telehealth? Telehealth refers to the use of digital communication tools, such as video calls, phone calls, text messaging, and online platforms, to provide healthcare services remotely. This technology allows patients to receive medical consultations, mental health support, follow-up care, and other health-related services without visiting a healthcare facility in person. While Telemedicine is often used interchangeably with Telehealth, Telemedicine specifically focuses on remote clinical services, whereas Telehealth encompasses a broader range of healthcare services, including administrative and educational support. Why is Telehealth Important? Several key factors have driven the rise of Telehealth: Increased Access to Care Telehealth removes geographic barriers, making it easier for individuals in rural or underserved areas to access high-quality care. Patients no longer have to travel long distances to see specialists or schedule an in-person visit, which can be especially beneficial for those with mobility issues, time constraints, or busy schedules. Convenience and Flexibility Telehealth offers patients the flexibility to schedule appointments from the comfort of their homes or workplaces, saving them time and reducing the stress of in-person visits. It also allows for more timely care, with many healthcare providers offering extended hours for virtual consultations. Cost-Effectiveness Telehealth can reduce the costs associated with in-person visits, such as transportation, parking, and time away from work. It also helps healthcare providers optimize their operations, allowing them to see more patients in less time, which can lower overall healthcare costs. Improved Continuity of Care For patients with chronic conditions or those requiring ongoing care, Telehealth enables better monitoring and follow-up care. Regular virtual check-ins help providers track progress and make necessary adjustments to treatment plans, all while maintaining a strong patient-provider relationship. The Benefits for Providers For healthcare providers, Telehealth offers numerous benefits that can enhance their practice: Expanded Patient Base With the ability to serve patients from across the country, Telehealth enables providers to expand their reach and serve more individuals. This is particularly advantageous for specialists who can offer their expertise to patients in remote locations. Reduced Overhead Costs By offering virtual consultations, providers can save on overhead expenses like office space, utilities, and staff required for in-person visits. This makes it possible to invest more in quality care and technology. Improved Patient Satisfaction Telehealth offers a more convenient and accessible experience for patients, which can lead to higher satisfaction rates. Happy patients are more likely to remain loyal to their healthcare providers and recommend them to others. Increased Efficiency Telehealth platforms allow providers to streamline their workflows by automating appointment scheduling, reminders, and patient intake forms. This results in less paperwork and fewer administrative tasks, freeing up time for more patient-focused care. Overcoming Challenges in Telehealth While Telehealth has made tremendous strides, it is not without its challenges. Some common barriers include: Technology Barriers Not all patients have access to the technology needed for virtual visits, such as smartphones, computers, or reliable internet connections. This can be a significant barrier, especially for elderly patients or those in low-income communities. Regulatory and Licensing Issues Telehealth services are subject to different regulations in each state or country. Providers must navigate a complex web of licensing requirements and reimbursement policies, which can be a challenge, especially for those offering cross-border services. Privacy Concerns Protecting patient data is a top priority in Telehealth. Providers must ensure that they comply with privacy regulations such as HIPAA in the United States to maintain patient confidentiality and avoid potential security breaches. Limitations for Certain Medical Conditions While Telehealth is ideal for routine consultations and follow-ups, it may not be suitable for patients who require physical examinations, lab tests, or imaging. In these cases, in-person visits are still necessary. The Future of Telehealth As technology continues to evolve, Telehealth is expected to become an even more integral part of the healthcare system. The future holds promising advancements, such as: Artificial Intelligence (AI) to assist in diagnosing conditions and providing personalized treatment recommendations. Remote Monitoring Devices that allow patients to track their health metrics (such as blood pressure, glucose levels, etc.) in real-time, which can then be shared with healthcare providers. Expanded Telehealth Services for specialties like physical therapy, dermatology, and even surgery consultations. With ongoing innovation and growing adoption by both healthcare providers and patients, Telehealth is poised to further revolutionize the way healthcare is delivered, making it more accessible, efficient, and patient-centered than ever before. Conclusion Telehealth has undoubtedly transformed the healthcare industry, providing solutions to some of its most pressing challenges. From increasing access to care to improving patient satisfaction and efficiency, Telehealth has become an essential tool in modern healthcare delivery. As technology continues to improve, its impact will only continue to grow, creating a future where healthcare is more personalized, accessible, and convenient for everyone.
How to Capture Images (Photos, Images), via the MyClinicMind Mobile App and Place Directly Into The Patient Chart
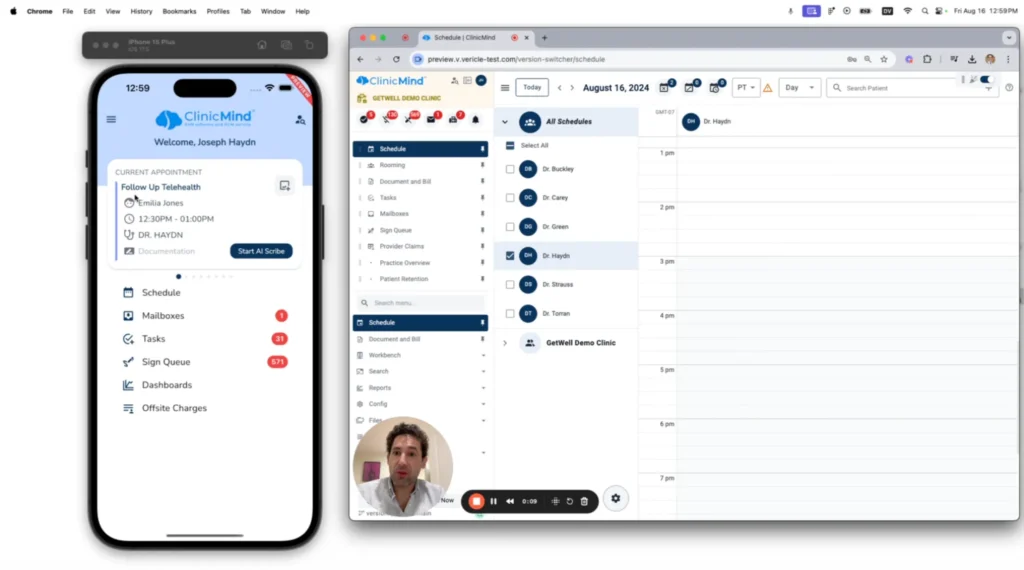
In this video, Dr. Roy Lirov demonstrates how to capture images using the UM ClinicMind mobile provider app. He walks through the process of adding images to a patient’s record, showcasing how easy it is to document visual information. Watch and learn how seamless it is to save and access images for patient records.
Patient Education and Meticulous Documentation
The Bedrock of a Thriving Chiropractic Practice The digital age has ushered in a new era for chiropractic care. While search engine optimization (SEO) effectively drives patients seeking relief from back pain and other musculoskeletal issues to your door, it often leaves them with a fragmented understanding of chiropractic treatment. Here’s where Dr. Evan Katz, a seasoned chiropractor and founder of Professionally Integrated, sheds light on the two pillars of a successful chiropractic practice: patient education and meticulous documentation. Building Trust and Empowering Patients Through Education Imagine a patient who finds your practice through a targeted SEO campaign. They likely have some knowledge of their back pain gleaned from online searches, but may lack a clear picture of how chiropractic care fits into their healing journey. Dr. Katz emphasizes the importance of going beyond simply addressing the symptoms. By educating patients about their specific condition, the underlying causes of their pain, and how chiropractic adjustments can address those root causes, you empower them to become active participants in their recovery. This fosters trust, improves treatment outcomes, and builds long-term patient relationships. Here are some key strategies chiropractors can utilize to effectively educate patients: Tailored Explanations: Ditch the medical jargon. Instead, take the time to break down complex medical concepts into clear, concise language that resonates with the individual patient’s level of understanding. Consider using visual aids like diagrams, animations, or even 3D models of the spine to enhance comprehension. Interactive Communication: Education is not a one-way street. Encourage patients to ask questions, express their concerns, and actively participate in discussions about their treatment plan. This open communication fosters trust and ensures patients feel comfortable and informed throughout the healing process. Role-playing potential scenarios can also be helpful, allowing patients to practice effective communication with employers or insurance companies regarding their chiropractic care. Patient-Centric Resources: Don’t let the education stop at your office door. Provide patients with informative handouts or access to online resources that explain their specific condition and chiropractic treatment options in detail. Consider creating a library of patient testimonials and success stories to showcase the positive impact of chiropractic care. This allows patients to revisit the information at their own pace, solidify their understanding, and feel a sense of community with others who have benefitted from chiropractic treatment. Safeguarding Your Practice and Patient Care: The Power of Detailed Documentation Detailed and accurate documentation isn’t just a box to tick; it’s a cornerstone of high-quality chiropractic care. Dr. Katz highlights how thorough documentation serves a dual purpose: protecting both chiropractors and their patients. It creates a clear and comprehensive record of the patient’s medical history, current symptoms, diagnostic test results (if applicable), the specific chiropractic techniques employed, the treatment plan, and the patient’s progress over time. This detailed record becomes invaluable, especially in personal injury cases, where it provides a clear timeline and factual evidence of the patient’s condition and treatment course. Here’s a deeper dive into what chiropractors should prioritize when documenting patient care: Comprehensive Patient History: This should include a detailed record of the patient’s medical background, current complaints and symptoms (including location, duration, and severity), any relevant risk factors (such as previous injuries, occupations, or lifestyle habits), and the results of any diagnostic tests performed (e.g., X-rays, MRIs). Clearly Defined Treatment Plan: Outline the specific chiropractic techniques you plan to utilize (e.g., spinal adjustments, soft tissue mobilization, physiotherapy), the frequency of adjustments (including any adjustments planned for future visits), and the overall treatment timeline with anticipated milestones for improvement. Detailed Progress Notes: Regularly update the patient’s file with objective observations about their progress. Include any changes in symptoms, including improvements or setbacks, the patient’s response to treatment (including any pain relief or increased mobility), and adjustments made to the treatment plan based on their progress. Empowering Chiropractors with Professionally Integrated Understanding the importance of thorough documentation is one thing, but implementing it efficiently within a busy practice can be another challenge. This is where Dr. Katz’s company, Professionally Integrated, comes in. Recognizing the time constraints faced by many chiropractors, Professionally Integrated offers a suite of resources and tools designed to streamline the documentation process. Their solutions allow chiropractors to efficiently capture and organize patient information using pre-populated templates, voice recognition software, and secure cloud storage options. This ensures meticulous records are maintained without sacrificing valuable treatment time with patients. Conclusion: A Sustainable Recipe for Success By prioritizing patient education and meticulous documentation, chiropractors can cultivate a thriving practice built on trust, informed patients, and successful treatment outcomes. Educated patients become active partners in their recovery, while strong documentation safeguards both patients and practitioners. By incorporating these practices, chiropractors can not only alleviate
Supercharge Chiropractic Patient Retention and Practice Growth
Let’s face it, retaining patients is a constant challenge in the chiropractic field. Studies show that the average new patient only visits 6 times before dropping off, and the national average for chiropractic retention rates hovers around a concerning 20%. But what if you could dramatically increase these numbers and build a thriving practice that thrives on patient loyalty? Dr. Miles Bodzin, a seasoned chiropractor with over 15 years of experience, has cracked the code on patient retention. By implementing these 5 key principles alongside Cash Practice, a comprehensive chiropractic management software, Dr. Bodzin not only improved patient satisfaction but also witnessed a significant surge in practice growth. Unveiling the Roadmap: Forecasting Care Imagine a patient walking into your office with a crick in their neck. They’re in pain, but they’re also anxious. How long will this take? How much will it cost? Dr. Bodzin emphasizes the importance of transparency. Instead of leaving patients in the dark, outline a clear care plan tailored to their specific needs. Visualize the Journey: Don’t rely solely on verbal explanations. Utilize charts, progress trackers, or infographics to visually represent the treatment timeline and milestones. This empowers patients to see the bigger picture and stay motivated. Breakdown the Costs: Be upfront about associated fees for each treatment stage. Consider offering flexible payment options or package deals to make chiropractic care accessible. Address Concerns: Openly discuss any potential roadblocks or setbacks patients may encounter during treatment. This proactive approach manages expectations and fosters trust. By providing a clear roadmap, you build trust and eliminate anxieties surrounding treatment duration and cost, leading to better patient engagement. Frictionless Flow: Streamlining Payments The last thing a patient experiencing pain wants to worry about is navigating a complex payment system. Make the payment process as smooth and invisible as possible. Automated Debits: Set up automatic debit options for patients who prefer a “set it and forget it” approach. This eliminates the need to remember recurring payments and ensures timely payments for your practice. Mobile App Integration: Integrate a secure mobile app into your practice. This allows patients to easily make payments directly from their phones, improving convenience and streamlining the process. Flexible Payment Gateways: Offer multiple payment options like credit cards, debit cards, or even health savings account (HSA) integration. This caters to patient preferences and makes chiropractic care more financially accessible. By minimizing friction at the payment stage, you improve patient experience and reduce the chances of them abandoning care due to financial concerns. The Power of Feedback: Keeping Patients Informed Patients often lack a clear understanding of how their treatment is progressing. Dr. Bodzin suggests implementing a “wellness score” system. This system translates complex medical data into an easy-to-understand format, like assigning A, B, C grades similar to a report card. Empowerment Through Visibility: Patients can see their progress objectively, leading to increased motivation and adherence to the treatment plan. Data-Driven Communication: Use the wellness score data to personalize patient communication. Highlight areas of improvement and celebrate milestones to keep patients engaged. Open Dialogue: The score system can spark conversations with patients, allowing you to address any concerns or questions they may have about their progress. This fosters a sense of partnership in their healthcare journey. Empowering patients with clear and regular feedback fosters a sense of partnership in their healthcare journey, leading to better long-term outcomes and improved retention. Stay Top-of-Mind: The Power of Frequent Communication In today’s fast-paced world, it’s easy for patients to forget about their ongoing chiropractic care. Regular communication keeps your practice name in front of them. Informative Email Newsletters: Develop engaging email newsletters with valuable content related to chiropractic health and wellness tips. Include patient success stories and practice updates to keep content fresh and interesting. Social Media Engagement: Utilize social media platforms like Facebook or Instagram to share educational content, patient testimonials, or behind-the-scenes glimpses into your practice. This allows you to connect with patients on a more personal level and build a sense of community. Personalized Outreach: Schedule automated appointment reminders and send follow-up messages after treatments. These messages express continued support and encourage patients to stay committed to their chiropractic care plan. By maintaining consistent and valuable communication, you stay top-of-mind and encourage patients to prioritize their ongoing chiropractic care. Convenience is King: Prioritizing Patient Experience Think of your favorite coffee shop. They offer comfy chairs, fast Wi-Fi, and maybe even a loyalty program. These small conveniences enhance your experience and keep you coming back for more. The same principle applies to your chiropractic practice. Online Appointment Scheduling: Allow patients to book appointments 24/7 through a user-friendly online platform. Extended Office Hours: Consider offering flexible appointment times, including evenings or weekends, to cater to busy schedules. Embrace New Technologies: Stay updated on the latest content creation tools like augmented reality (AR) or virtual reality (VR) and see if they can be integrated into your blog for a truly unique experience.
Embracing Healthy Longevity
Healthy longevity isn’t just a buzzword anymore; it’s a national focus backed by significant investments and collaborations across various sectors. With organizations like the National Academy of Sciences, AARP, and government agencies rallying behind the cause, the pursuit of a thriving, extended lifespan is gaining momentum. Recently, I had the privilege of sitting down with Dr. Eric Plasker, a prominent figure in the world of chiropractic care and longevity, to discuss the latest venture in promoting healthy longevity through a collaborative effort with Life University and Genesis. A Collaboration for Change: Dr. Plasker kicks off our conversation by highlighting the collaborative effort between the 100 Year Lifestyle and Life University, presenting a new seminar titled “Healthy Longevity and Chiropractic: From Birth to 100 Years and Beyond.” This seminar aims to delve into the importance of chiropractic care throughout all stages of life and how it contributes to healthy longevity. With a blend of informative sessions and practical implementation strategies, the seminar promises to empower chiropractors to lead the healthy longevity movement in their communities. Stories of Transformation: Throughout our discussion, Dr. Plasker shares compelling stories of individuals whose lives have been transformed through chiropractic care and lifestyle interventions. From a 60-year-old soccer player winning national championships to uncovering the root causes of health issues dating back to birth, these stories underscore the profound impact of proactive healthcare practices on longevity and well-being. Business Perspectives: Beyond the realm of healthcare, our conversation extends to the business side of promoting healthy longevity. Dr. Plasker emphasizes the importance of building lifetime relationships with patients and leveraging modern tools like Genesis software to streamline practice management. This collaboration isn’t just about delivering healthcare; it’s about amplifying the profession’s impact through purpose-driven partnerships. Authentic Collaboration for Impact: What sets this collaboration apart is its authenticity and shared vision for empowering individuals to live vibrant, fulfilling lives at every age. Dr. Plasker and I discuss the significance of aligning values and collaborating with like-minded partners to drive meaningful change. It’s not just about promoting services; it’s about fostering genuine connections and creating lasting impact in communities. Looking Ahead: As we wrap up our conversation, Dr. Plasker invites chiropractors and healthcare professionals to join the upcoming seminar in May, promising a transformative experience that will reshape both their practices and perspectives. With a focus on touching, moving, and inspiring participants, this seminar represents a pivotal moment in the journey towards healthy longevity and holistic well-being. Conclusion: The pursuit of healthy longevity is a collective endeavor that transcends individual disciplines and institutions. Through authentic collaboration, purpose-driven partnerships, and a commitment to lifelong well-being, we can pave the way for a future where every individual has the opportunity to thrive, from birth to 100 years and beyond. Join us on this journey towards a healthier, more vibrant world. Watch the full episode here.
WebExercises and Remote Therapeutic Monitoring
Welcome back, Genesis Nation! Today, we’re diving into a game-changing integration that is transforming the landscape of chiropractic care. We have the pleasure of hosting Dr. David Cruz, the mastermind behind Web Exercises, a platform designed to seamlessly integrate exercise prescription with chiropractic care. But that’s not all; we’re also exploring the exciting world of Remote Therapeutic Monitoring (RTM), a potential game-changer for chiropractors seeking to validate and bill for their services remotely. The Birth of WebExercises: In our conversation with Dr. Cruz, we learned about the genesis of Web Exercises. It all started 15-16 years ago when Dr. Cruz, a self-proclaimed movement geek, recognized the powerful synergy between chiropractic care and exercise. The challenge was to find a way to engage patients beyond the confines of the chiropractic office. Enter Web Exercises – a platform that allows healthcare providers, including chiropractors, to create, send, and remotely monitor personalized exercise programs for their patients. The Integration with Genesis: The beauty of Web Exercises lies in its seamless integration with Genesis chiropractic software. Dr. Cruz demonstrated how chiropractors can effortlessly access and incorporate exercise programs into their patient documentation. With just a few clicks, exercises tailored to a patient’s specific needs and conditions can be added to their profile, ensuring continuity of care beyond the chiropractic office. Creating Tailored Exercise Programs: Dr. Cruz showcased the user-friendly interface of Web Exercises, making it easy for chiropractors to create personalized exercise programs. Whether addressing low back pain, neck issues, or postural concerns, the platform offers an extensive library of exercises searchable by keywords, body regions, equipment, and more. Additionally, pre-built protocols and evidence-based exercise recommendations further streamline the process. The Chiropractic Mirror Image Library: For chiropractors utilizing Chiropractic BioPhysics (CBP) or those seeking mirror image exercises, Web Exercises offers a specialized library. This feature enables chiropractors to choose exercises that align with CBP principles, ensuring a comprehensive approach to patient care. Remote Therapeutic Monitoring (RTM): Dr. Cruz provided a sneak peek into the evolving landscape of Remote Therapeutic Monitoring (RTM). This emerging trend allows healthcare providers, including chiropractors, to bill for creating, sending, and remotely monitoring patients’ musculoskeletal information. While the field is still navigating regulatory nuances, early signs indicate that RTM could become an industry standard, allowing chiropractors to be reimbursed for the valuable services they provide remotely. Conclusion: Our discussion with Dr. Cruz has shed light on the impactful intersection of chiropractic care and exercise prescription. Web Exercises, coupled with the potential of Remote Therapeutic Monitoring, opens new doors for chiropractors to enhance patient outcomes and streamline their practices. As we continue to explore the evolving landscape of healthcare, innovations like Web Exercises are paving the way for a future where movement truly matters in holistic patient care. Stay tuned for more updates and insights from Genesis Nation!
No-Show Risk Management

When patients miss appointments, they interrupt the flow of patient care, impede clinic productivity, and signal an eroding patient loyalty. The rate of no-shows runs at 30% for the average family practice. A missed appointment amounts to missed billing revenue. Worse, if clinicians are part-time or full-time staff rather than contracted, they sit idle on the company clock, losing money with each passing minute. Finally, a missed appointment could be a symptom of a deserting patient, signaling a potential loss of long-term billing revenue. Most clinics lose an average of 20% of their revenue due to missed appointments. Lost revenue may not be the largest problem caused by no-shows. Other problems span health damage, patient liability risks, reduced accessibility, and impeded resident education. Rigorous no-show management methods using advanced technologies integrate scheduling and billing data, reduce no-show rates, and improve associated revenues by more than 50%. They also mention the comparable improvement of long-term patient loyalty (Hashim et al., 2001). No-Show Impact on the Clinic Figure 1. No-Show Impact (Hayhurst, AthenaHealth) A missed appointment poses five kinds of problems: Health damage – A patient’s health can be damaged due to interrupted continuity of care or a missed opportunity to solve an acute health problem. The doctor also loses an opportunity for a timely review of patient health, treatment progress, etc. Liability risk – A patient who misses an appointment and suffers an injury may have a viable cause for a lawsuit against the practice. To avoid such risk, the doctor must maintain evidence of giving clear directions and making reasonable efforts to ensure the patient’s compliance with the care program, including keeping follow-up appointments. Reduced accessibility – Other patients are postponed and don’t get access to care because of a no-show or canceled appointment. Impedance to medical education – A resident or intern misses an opportunity to learn and improve care skills. Loss of revenue – The clinic cannot make up revenue due to missed appointments. A financial impact arises from wasted resources, such as staff time, equipment, and facility utilization, that were allocated for the no-show patient. No-Show Frequency Distribution No-show rates average about 20%: 10% of clinics have less than 10% no-shows, 42% of clinics have 10%–20%, 34% of clinics have 20%–30%, and 14% of clinics have more than 30% no-shows (Izard, 2005). Further, the top 10 clinics regarding the lowest no-show rates range from 3%–9% for no-shows, while the bottom ten clinics reach 33%–57% (Moore et al. 2001). Common reasons behind No-show Forgetfulness: Patients may simply forget about their appointments due to a busy schedule, lack of reminder systems, or cognitive factors. Transportation issues: Lack of transportation or difficulty accessing reliable transportation can prevent patients from attending appointments. Fear or anxiety: Some patients may experience fear or anxiety related to medical procedures, test results, or hospital settings, leading them to avoid or cancel their appointments. Financial constraints: Financial limitations, such as the inability to afford healthcare services or medications, may result in patients skipping or postponing appointments. Illness or emergencies: Patients may have unexpected illnesses or emergencies that prevent them from attending their scheduled appointments. Lack of awareness or understanding: Patients may not fully comprehend the importance of their appointments or the consequences of missing them, particularly for follow-up care or chronic conditions. Language and cultural barriers: Language barriers or cultural differences can impede effective communication and understanding, leading to missed appointments. Long waiting times: Lengthy wait times at hospitals can discourage patients from attending appointments, particularly if they have competing priorities or other time constraints. Stigma or fear of judgment: Patients with certain medical conditions or mental health issues may experience stigma or fear of judgment, causing them to avoid seeking care or attending appointments. Personal or work-related conflicts: Conflicts arising from personal commitments, work schedules, or other obligations may interfere with appointment attendance (Marbouh et al., 2020). The image below shows common reasons for missed appointments (Saif et al., 2018). According to a study, among all patients, those who never have a no-show appointment have an attrition rate of slightly less than 19 percent. In contrast, almost 32 percent of patients with one or more no-shows do not return to the same practice within 18 months (Hayhurst, AthenaHealth). Three-Phase No-Show Management Strategy An effective no-show management strategy is based on tracking, rescheduling, and follow-up: Tracking Record all no-shows and reconcile them with billing daily. Record no-show reasons and follow-up notes in patient records. Review end-of-day reports daily. Rescheduling in real-time Allow patients to request appointments online using the Internet Overbook and use waiting lists. Fill new openings with walk-ins or patients from the waiting list. Follow-up Activate a sequence of reminder calls/emails to all patients ten days, two days, and one day before their appointments. Place follow-up calls to determine reasons for no-shows and reschedule the patients. Reminder calls for upcoming appointments and follow-up calls on recent no-shows are effective strategies for billing revenue protection because they reduce the number of no-shows and help early identification of incipient patient attrition and other patient-related problems (Hashim et al., 2001). Follow up with warning letters after one no-show. Dismiss patients from the practice after three no-shows. Reminder calls or emails before an appointment remains the most effective method to prevent missed appointments. Additionally, sending reminders via email and allowing patients to confirm online turns an office reminder into a patient’s action item, significantly outperforming the impact of a voice message or postcard. While recognizing the benefits of reminder calls, busy practice owners often neglect or postpone reminder and follow-up calls because of other office management priorities, such as personnel issues or billing. As with any other management initiative, a reminder call strategy must be implemented systematically and consistently to get results. Note that outsourcing reminder calls to calling services and using the Internet reduce the cost of reminders. Therefore, reaching all patients before their appointments makes good business sense. Ways to reduce No-shows Automation of appointment reminders: Implementing automated appointment reminders can significantly reduce

