Pain in the ASSessment
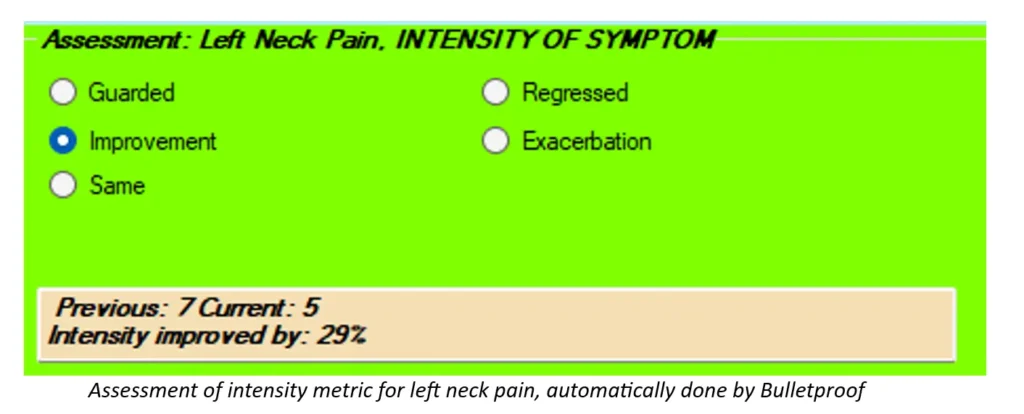
There’s ONE part of our SOAP notes that I’ve been preaching about for years, but it seems as though not many doctors are paying close enough attention to it. It’s the Assessment. Here’s what I see in most records that I review in the Assessment part of the SOAP Note: “Patient is responding well to care.” “Patient is the same.” “Patient is responding slower than expected.” To begin with, according to our friends at Centers for Medicare and Medicaid Services (CMS), we are to document an assessment for each condition that we are treating. If we’re treating a patient for headaches, neck pain and upper back pain, we need to document an assessment for each of these. Even though I’m talking about Medicare, and you may see very few Medicare patients, just remember that Medicare creates the rules that most insurers (and even state boards) follow. If we document well for Medicare, we’re that much closer to the promised land. OK, back to my point. The next thing that Medicare is looking for in the Assessment is how each condition is on today’s visit as compared to the previous visit. That can be problematic. Do they really expect us to look back a visit every time the patient comes in and we have to compare that visit to today’s visit? And what if, on the previous visit, we said something like “Patient presents with neck pain” and on today’s visit we write, “Patient presents with neck pain.” See the problem? Then Medicare wants us to document the effectiveness of our treatment for each condition as compared to the previous visit. Seriously? If you’ve been reading my previous blog posts, you’ll remember that I’m making a big deal about us using certain metrics with our documentation. By using these metrics, we can actually document how each condition is responding since the previous visit AND the effectiveness of our treatment. That’s easy with the right technology. I recently looked at notes from an Administrative Law Judge in a Medicare audit. The particular doctor being audited did a pretty good job of documenting P.A.R.T. and most likely thought he was in the clear. Not so much. The judge noted, for all claims audited, that the doctor failed to document how each condition had changed since the previous visit AND the effectiveness of treatment. Medicare wants their money back – the tune of TENS of THOUSANDS of DOLLARS. If there are any complicating factors, specific to each condition, that may slow the patient’s recovery for that condition, we can document those, too. I make sure that these complicating factors appear on every visit in my SOAP notes. Finally, we can document the diagnoses under Assessment. It really doesn’t matter where in your soap notes you put the diagnoses, but Assessment seems to be the most logical. You’ll want to document both the ICD10 code AND the description, though, not one or the other. Instead of thinking about the Assessment as a pain in the ASSessment, we can think differently about it so we can use it in our favor – by showing the world how awesome chiropractic is and how effective our treatment is – both quantifiably and functionally. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
Documenting the Daily Objective Findings
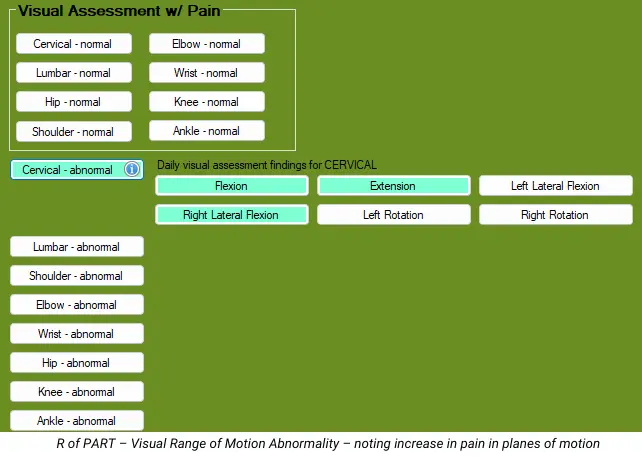
There seems to be some confusion among chiropractors as to what objective findings we need to document on our daily visits. I, and others, have been teaching for a number of years to follow the PART format of documentation for ALL of our patients. This PART format is what is REQUIRED by Medicare, and, to be honest, it works quite well for ALL of our patients. So, let’s review what PART is. The P of PART stands for Pain/Tenderness. As I wrote in a previous article, documenting the metrics of pain intensity and pain frequency will satisfy this component of PART, and it gives us two metrics we can track over time. The A of PART stands for Asymmetry/Misalignment. For this, there are 3 categories: posture, gait and restriction/subluxation. We only are required to document ONE of these, and, if you plan on adjusting your patient, I recommend choosing the restriction/subluxation to document, which makes posture and gait optional. The R of PART stands for Range of Motion Abnormality. No one expects us to actually measure range of motion on every visit – we can save that for the exams. On the daily visits, though, we can simply do a visual assessment of range of motion, noting if there is an increase in pain for each plane of motion or not. Don’t make up fake measurements – there’s no need to do that here. If cervical flexion increases the pain when compared to neutral, it’s positive. That’s it. The T of PART stands for Tissue/Tone Changes. Quit talking about the paraspinal muscles here. Instead, be more specific for the muscles, like left trapezius, right levator scapulae, bilateral supraspinatus, etc. There’s no requirement to grade the spasms or trigger points – just note which muscles are involved. Medicare then tells us that we don’t necessarily have to document all four of these on each visit, but that we HAVE to document at least 2 of the 4, with 1 of the 2 being Asymmetry/Misalignment or Range of Motion Abnormality. To make this easier (hopefully), we need to make sure that everything we do from a treatment perspective must be justified by what you documented as your findings for that visit. For example, if you are doing passive modalities on your patients, like hot packs and electrical muscle stimulation, you’re probably doing that to decrease pain and muscle spasms/trigger points. Make sure that you’ve documented pain and spasms in your notes. If you’re performing manual therapy on a patient, you’re probably doing that to relieve pain and muscle spasms/trigger points. Make sure you’ve documented that. If you’re having your patients perform therapeutic exercises, you’re probably doing that to decrease pain with certain motions and improve function. Make sure you’ve documented that. But here’s one that’s been catching my attention lately in the many record reviews I perform each month. I’m talking about the spinal and/or extremity restrictions/subluxations. Too many of you are documenting the segments you adjusted but are NOT documenting the restrictions/subluxations in your objective findings. You may be thinking it’s implied or assumed, but it’s NOT. As a reviewer, I assume nothing. What you’ve documented is what you’ve documented. If you documented that you adjusted C3, C5, T4 and L1 but you did NOT document that there were restrictions with those segments, I will point out that you did not document a justification for those adjustments. So, here’s how it could look: You perform spinal adjustments and hot packs and electrical muscle stimulation – you need to document the pain (P intensity and frequency), spinal restrictions/subluxations (A) and muscle spasms/trigger points (T). You perform spinal adjustments and manual therapy – you need to document the pain (P), spinal restrictions/subluxations (A) and muscle spasms/trigger points. You perform spinal adjustments and therapeutic exercises – you need to document the pain (P), spinal restrictions/subluxations (A) and increased pain with certain planes of motion (R). You perform spinal adjustments, manual therapy and therapeutic exercises – you need to document the pain (P), spinal restrictions/subluxations (A), increased pain with certain planes of motion (R) and muscle spasms/trigger points (T). That way, every treatment that you perform is justified in your notes. In my EMR, when I document the spinal/extremity restrictions in my objective findings and then click on spinal/extremity adjustments in my treatment plan, the restrictions from my objective findings automatically populate, and the same goes for manual therapy and therapeutic exercise. This is how I blend exceptional documentation with technology to create a great and compliant SOAP note in the least amount of time. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
Documentings Musta, Shoulda, Coulda, Part 2

In my last article, I discussed the MUSTs and the SHOULDs of Subjective Documentation, that being Pain Intensity, Pain Frequency and the use of Outcome Questionnaires. Now we’ll tackle the Objective Findings. Even though many chiropractors don’t treat a lot of Medicare patients, please understand that Medicare creates many of the rules. I’ve seen other commercial payors using the Medicare documentation guidelines for their policies, which actually makes it easier for us. Medicare does a great job of narrowing down which objective findings they’re looking for, as part of their PART requirements. The first component of PART is P – Pain and Tenderness, which can fall under the Subjective complaints we discussed in the last article. The next component is A – Asymmetry/Misalignment. Medicare tells us that this includes Posture, Gait and Subluxation/Restriction. Let’s start with the MUSTs. If you plan on performing a chiropractic adjustment/manipulation, you MUST document a reason for it, which would be the subluxation/restriction. This applies to both the spine and extremities. Medicare doesn’t care how we find these subluxations/restrictions, but they do care how we document them. They DON’T want us documenting subluxations/restrictions in regions, such as “cervical, thoracic, lumbar.” They REQUIRE us to document the specific segments, though, such as “C3, T4 and L5.” There is no requirement to document specific spinal listings. They do give another option, though, for when the subluxation/restriction crosses two areas. For example, we can document occiput and C1 or atlanto-occipital. We can document C7 and T1 or cervicodorsal. We can document L5 and S1 or lumbosacral. When I review personal injury records, some chiropractors like to document that they found subluxations/restrictions at literally EVERY level of the spine. That tends to be an “eye roller.” We can be more specific than that. If your treatment centers around posture or gait, and not the subluxations/restrictions, you can document these instead, which makes documentation of the subluxations/restrictions optional, as long as you’re not performing chiropractic adjustments/manipulations. The next component of PART is R – Range of Motion Abnormality. According to the 1997 HCFA/AMA Guidelines for the Musculoskeletal System, all the E/M exam requires is a visual assessment of range of motion noting PAIN, or a palpatory assessment noting crepitation or contracture. For this part of this exam, measured range of motion is NOT required. However, if you want to use range of motion as an outcome assessment to monitor the patient’s progress, you’ll need to measure the range of motion. I don’t mean doing a visual assessment and making up a number – I mean actually measuring the range of motion. Are range of motion measurements a good outcome assessment? Sometimes it is, and sometimes it’s not. If your patient says they feel like they’re not moving well, or if you observe that they’re not moving well, measuring range of motion can be a decent outcome assessment. Make sure when you document this that you mention that you actually measured the range of motion (dual inclinometers for spine, goniometer for extremities) and document what the normal values are (AMA Guides are the most accepted). At re-exams, note the new measurements and if each planed of motion showed improvement, regression or no change, and by how many degrees/percent. Next is the T of PART, which is Tissue/Tone Changes. Don’t document “paraspinal muscles” for this – it’s too vague and tends not to change. Instead, document more specific muscles (i.e. trapezius, levator scapulae, etc.) and if it’s left, right or bilateral. Keep in mind that muscle spasms tend to be more acute in nature, while trigger points can be more chronic. As the patient progresses, make sure you change these to reflect their improvement (or lack of). Do we need to document all four components of PART? Not necessarily, according to Medicare. They require us to document at least 2 of the 4, but 1 of the 2 MUST be A or R. But let’s think of this more practically. If your patient has 1 or more symptoms, document the P of PART with pain intensity and pain frequency for each condition, and an outcome questionnaire for each condition at the first visit and then every 2 weeks. If you plan on adjusting your patient, you MUST document the A (restriction/subluxation) for each segment of the spine/extremity that’s restricted. If you DON’T plan on adjusting the patient, you can document the R. On a typical daily visit with no exam, all you need to do is perform a visual assessment of range of motion noting if there is an increase in pain in each plane of motion. At re-exams, you can measure the range of motion to monitor the patient’s progress. If you plan on performing Therapeutic Exercises with the patient, you’ll want to document the planes of motion that increased pain (R of PART). If you plan on performing Manual Therapy on the patient, you’ll want to document in which muscles you found spasms/trigger points. In other words, you MUST justify ALL of your treatment with your objective findings. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
Documentings Musta, Shoulda, Coulda, Part 1
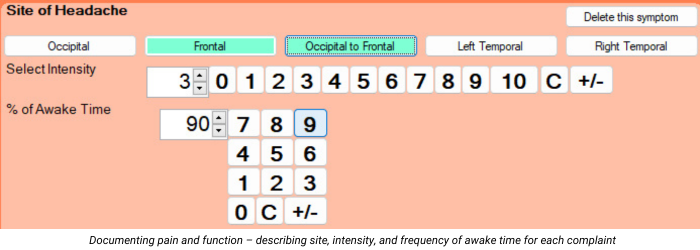
Let’s face it. With regards to our documentation, some doctors don’t say enough, while other doctors say too much. So which is better? Let’s narrow this down to the big three: The Must, the Should and the Could. There are some things we MUST document. They’re required components and if we miss them, we’re toast. Then there are certain things that we SHOULD document. These things aren’t exactly required, but they really enhance our documentation. And then there’s the COULD. There are plenty of things we COULD document, but I’m telling you – most of these are a COMPLETE WASTE OF TIME. Now, if it means a lot to you, ‘cause you just want to say it, well, OK. As long as you know, though, that from a documentation perspective, NO ONE BUT YOU CARES! They aren’t required, they don’t add anything to your documentation and they are just wasting your valuable time. Believe it or not, I want you to document LESS. But the things I want you to document are only the MUSTS and the SHOULDS. Let’s kick the COULDS to the proverbial curb. So what are the MUSTS? Let’s start with what Medicare REQUIRES. I’ve talked about this before: JUST TWO THINGS. And they are…Pain and Function. Everyone wants those same two things. All of the guidelines that are used against us, which we can use FOR us, want these 2 things – for ALL patients. Starting with the Subjective part of SOAP, the first MUST is to document each condition that you’ll be treating. For the purposes of this article, let’s limit it to musculoskeletal. Be specific without going too far. For example, documenting “headache” isn’t enough. We could document “occipital headache.” For neck pain, upper back/middle back/low back pain, we could say “neck/upper back/middle back/low back”, or we can document “neck on the left/upper back on the right/middle back on the left/low back on the right.” Without saying left or right, we’re implying that the pain is not off to one side. The next Subjective Must is the Pain Intensity of each symptom. All of the guidelines want us to have our patients rate their pain, typically from 1-10, with 10 being the worst. The days of documenting simply “neck pain” are over. Here’s an easier way to think of this. Ask the patient, for each condition, if they would call it “mild, moderate or severe.” Most people sort of understand that. Here’s what you need to know: mild is 1-3, moderate is 4-7 and severe is 8-10. If the patient says their pain is MILD, ask them to give you a number between 1 and 3, with 3 being the worst. This tends to make it much easier for the patient to come up with a number. The next Subjective Must is the use of outcome questionnaires. Don’t roll your eyes. This is the easiest, fastest and least expensive outcome assessment we can use. It’s a way that we can effectively track our patients’ progress with regard to their function. Better yet, ALL of the various guidelines want this. It’s also required by Medicare. There are valid and reliable outcome questionnaires for practically every musculoskeletal body part. All we need to do is give the patient ONE questionnaire for each condition that we’re treating. Some of you have been using the Revised Oswestry for low back pain and the Neck Disability Index for neck pain, both which are fine. I prefer the Neck Bournemouth Questionnaire and the Back Bournemouth Questionnaire, since these are only 7 questions each, meaning they’re faster and easier for patients to complete, and they also have a psychosocial question, which is missing from Oswestry and NDI. There’s a great headache questionnaire and several questionnaires for the upper and lower extremities. At the very minimum, we should have the ACTIVE patient complete the questionnaires on the FIRST visit and then “every 30 days or sooner”, which is what Medicare requires. Now let’s talk about the Subjective SHOULD. The first SHOULD is Pain Frequency. I talked about this in my last article. While not required, it can add SO MUCH to our documentation, especially if the pain intensity isn’t changing very quickly. The best way to document this FREQUENCY is with an actual percentage of awake time. Stick to 5 or 10% increments, like 50%, 75%, 100% and so on. Your documentation is MUCH better if the intensity is stuck at a 6/10 for 5 visits, but the frequency goes from 100%, to 95%, to 85%, to 80%, to 75%. This is also MUCH better than saying “occasional, intermittent, frequent and constant.” While they’re better than not saying anything, they still suck because your patient can be stuck in the constant range for 2 months and your documentation looks like they’re not getting any better. The next Subjective SHOULD is how often we have the patient complete the outcome questionnaires. I mentioned above that Medicare requires that we have the patients complete these “every 30 days of sooner.” However, I recommend that we do these questionnaires EVERY 2 WEEKS, so we can see and track the patient’s progress. Another reason for the every 2 week re-assessment is that several of the guidelines say “if the patient does not show signs of objective improvement in any two successive two week period, referral is indicated.” I know, these outcome questionnaires are subjective and not objective, but that’s not what they mean. They just want to see measurable and functional improvement. If there’s no measurable and functional improvement after 2 weeks, you can change something about your treatment and go for another 2 week trial of care. As long as you’re showing improvement, you’re good. As long as you’re showing that you’re changing the treatment after no improvement, you’re good – at least for another 2 weeks. These Subjective MUSTS and SHOULDS let us document in terms of METRICS. Tracking these numbers will enable us to show how each metric is changing over time with our treatment. It will also enable us to document specific treatment goals which will make our documentation exceptional. But…have you ever had the experience when the patient tells you something that can’t quite fit into a metric? For example, I heard this the other day: “My pain went to a 0 after my last visit, and it lasted for

