Let’s face it. With regards to our documentation, some doctors don’t say enough, while other doctors say too much. So which is better?
Let’s narrow this down to the big three: The Must, the Should and the Could. There are some things we MUST document. They’re required components and if we miss them, we’re toast.
Then there are certain things that we SHOULD document. These things aren’t exactly required, but they really enhance our documentation.
And then there’s the COULD. There are plenty of things we COULD document, but I’m telling you – most of these are a COMPLETE WASTE OF TIME. Now, if it means a lot to you, ‘cause you just want to say it, well, OK. As long as you know, though, that from a documentation perspective, NO ONE BUT YOU CARES! They aren’t required, they don’t add anything to your documentation and they are just wasting your valuable time.
Believe it or not, I want you to document LESS. But the things I want you to document are only the MUSTS and the SHOULDS. Let’s kick the COULDS to the proverbial curb.
So what are the MUSTS? Let’s start with what Medicare REQUIRES. I’ve talked about this before: JUST TWO THINGS. And they are…Pain and Function. Everyone wants those same two things. All of the guidelines that are used against us, which we can use FOR us, want these 2 things – for ALL patients.
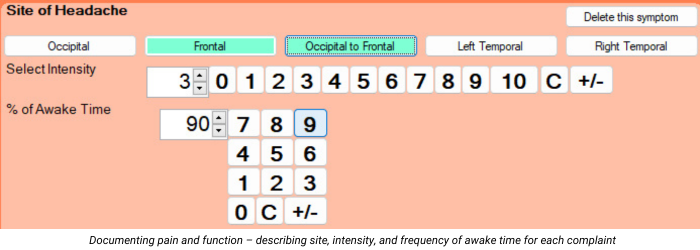
Starting with the Subjective part of SOAP, the first MUST is to document each condition that you’ll be treating. For the purposes of this article, let’s limit it to musculoskeletal. Be specific without going too far. For example, documenting “headache” isn’t enough. We could document “occipital headache.” For neck pain, upper back/middle back/low back pain, we could say “neck/upper back/middle back/low back”, or we can document “neck on the left/upper back on the right/middle back on the left/low back on the right.” Without saying left or right, we’re implying that the pain is not off to one side.
The next Subjective Must is the Pain Intensity of each symptom. All of the guidelines want us to have our patients rate their pain, typically from 1-10, with 10 being the worst. The days of documenting simply “neck pain” are over. Here’s an easier way to think of this. Ask the patient, for each condition, if they would call it “mild, moderate or severe.” Most people sort of understand that. Here’s what you need to know: mild is 1-3, moderate is 4-7 and severe is 8-10. If the patient says their pain is MILD, ask them to give you a number between 1 and 3, with 3 being the worst. This tends to make it much easier for the patient to come up with a number.
The next Subjective Must is the use of outcome questionnaires. Don’t roll your eyes. This is the easiest, fastest and least expensive outcome assessment we can use. It’s a way that we can effectively track our patients’ progress with regard to their function. Better yet, ALL of the various guidelines want this. It’s also required by Medicare. There are valid and reliable outcome questionnaires for practically every musculoskeletal body part. All we need to do is give the patient ONE questionnaire for each condition that we’re treating. Some of you have been using the Revised Oswestry for low back pain and the Neck Disability Index for neck pain, both which are fine. I prefer the Neck Bournemouth Questionnaire and the Back Bournemouth Questionnaire, since these are only 7 questions each, meaning they’re faster and easier for patients to complete, and they also have a psychosocial question, which is missing from Oswestry and NDI. There’s a great headache questionnaire and several questionnaires for the upper and lower extremities. At the very minimum, we should have the ACTIVE patient complete the questionnaires on the FIRST visit and then “every 30 days or sooner”, which is what Medicare requires.
Now let’s talk about the Subjective SHOULD. The first SHOULD is Pain Frequency. I talked about this in my last article. While not required, it can add SO MUCH to our documentation, especially if the pain intensity isn’t changing very quickly. The best way to document this FREQUENCY is with an actual percentage of awake time. Stick to 5 or 10% increments, like 50%, 75%, 100% and so on. Your documentation is MUCH better if the intensity is stuck at a 6/10 for 5 visits, but the frequency goes from 100%, to 95%, to 85%, to 80%, to 75%. This is also MUCH better than saying “occasional, intermittent, frequent and constant.” While they’re better than not saying anything, they still suck because your patient can be stuck in the constant range for 2 months and your documentation looks like they’re not getting any better.
The next Subjective SHOULD is how often we have the patient complete the outcome questionnaires. I mentioned above that Medicare requires that we have the patients complete these “every 30 days of sooner.” However, I recommend that we do these questionnaires EVERY 2 WEEKS, so we can see and track the patient’s progress. Another reason for the every 2 week re-assessment is that several of the guidelines say “if the patient does not show signs of objective improvement in any two successive two week period, referral is indicated.” I know, these outcome questionnaires are subjective and not objective, but that’s not what they mean. They just want to see measurable and functional improvement. If there’s no measurable and functional improvement after 2 weeks, you can change something about your treatment and go for another 2 week trial of care. As long as you’re showing improvement, you’re good. As long as you’re showing that you’re changing the treatment after no improvement, you’re good – at least for another 2 weeks.
These Subjective MUSTS and SHOULDS let us document in terms of METRICS. Tracking these numbers will enable us to show how each metric is changing over time with our treatment. It will also enable us to document specific treatment goals which will make our documentation exceptional.
But…have you ever had the experience when the patient tells you something that can’t quite fit into a metric? For example, I heard this the other day: “My pain went to a 0 after my last visit, and it lasted for 2 hours. Then the pain increased to a 4, and then to a 5, which is where it is today.” For that kind of circumstance, I’ll still document the Intensity and Frequency with the metrics, but I’ll type in a sentence (no need to over do it) explaining that. This doesn’t need to happen on every visit, just when your patient says something that you think will offer more context to your documentation. Reviewers like me would love to see that from time to time.
Gregg Friedman, DC, CCSP, FIACA
Creator of The Bulletproof Chiro EMR