ClinicMinders make our company what it is. We hire for attitude over experience and we pride ourselves on attracting and retaining people with COURAGE.
COURAGE to stick to our Core Values and help providers remain independent and grow. We also believe in radical transparency, so we publicly share Core Values with anyone who is interested in our approach to work. This fanatical focus is more than a mantra; it is evident in our software, our support, and the services we keep adding. And doing so makes us ecstatic.
ClinicMind offers great benefits, an attentive team, and a flexible and professional work environment
ClinicMind offers a work-from-home (WFH) employment structure for work-life balance and professional growth. WFH benefits promote job satisfaction, family focus, and productivity.
ClinicMind leverages its access to the global talent pool and fosters a strong remote company culture through adherence to the core values of excellence, learning, and teamwork.

Role Overview
ClinicMind is hiring a founding Marketing Director to build and run a predictable lead engine. This is a hands-on, outcomes-owned role that turns Growth Strategy into weekly execution across paid ads, events, content/SEO, and partner motions—leveraging agencies and contractors early, then hiring internally as ROI proves capacity needs.
You’ll partner closely with Edisa (Chief Growth Strategy Officer) and Sales leadership to improve lead volume, lead quality, and conversion from first touch to SQL to opportunity—through clear accountability, fast iteration, and disciplined execution.
In addition to demand generation, this role is accountable for maintaining ClinicMind’s market credibility and brand leadership, including third-party trust signals (e.g., G2) and customer proof that converts into demand. ClinicMind also expects marketing to lead by example, using PatientHub internally as the default system for marketing/sales workflows—so we can credibly show customers how to replace fragmented tools with one platform.
Primary Accountability
Deliver a scalable, measurable marketing system that produces a qualified pipeline for Sales while strengthening ClinicMind’s brand leadership and credibility in-market.
Core Success Metrics (owned by this role)
New logo: deliver SQL volume aligned to Sales goals (targets discussed in interview)
Efficiency: maintain all-in cost per SQL while scaling
Quality: improve MQL → SQL, SQL → Opportunity, and downstream show/hold rates (in partnership with Sales/SDRs)
Predictability: weekly dashboard and attribution clarity by motion/channel
Brand leadership: sustain and grow third-party credibility (e.g., G2 presence, review velocity/quality, proof-point packaging)
PatientHub-first execution: ensure ClinicMind marketing/sales workflows run on PatientHub; internal learnings become external proof + enablement
Core Responsibilities
Build and operate the lead engine
Own the end-to-end marketing system that delivers new logo SQLs aligned to Sales goals
Define and manage distinct lead pools (new logo vs existing customers; paid vs organic vs events vs lifecycle), with clear attribution and conversion reporting by pool.
Translate Growth Strategy into a clear quarterly plan and a weekly execution cadence (launches, experiments, optimizations)
Maintain a performance portfolio across channels and reallocate budget based on cost/SQL, SQL → Opportunity, and win-rate signals
Own CRM hygiene for marketing-owned stages (definitions, routing rules, dedupe, SLA reporting) in PatientHub.
Run multi-channel demand gen with speed and discipline
Plan and launch campaigns across paid, content/SEO, email/lifecycle, webinars, and events—focused on qualified demand, not vanity metrics
Build and optimize landing pages, offers, nurture sequences, and conversion paths (with internal and agency support)
Create a repeatable “campaign factory” process: brief → build → QA → launch → measure → iterate
Manage agencies and contractors like an internal team
Lead agencies/contractors across paid media, creative, SEO, web, and content with clear briefs, KPIs, timelines, and performance reviews
Ensure vendor output ties directly to pipeline outcomes; cut or correct underperformance fast
Establish standards for messaging consistency, design quality, and delivery quality across all vendor work
Improve lead quality and sales conversion with tight handoffs
Partner with Sales/SDRs to define and refine lead definitions, scoring, routing, and SLAs
Improve conversion at each stage: MQL → SQL, SQL → Opportunity, show/hold rates, and downstream pipeline contribution
Build enablement assets (talk tracks, one-pagers, case studies, sequences) that increase conversion and shorten sales cycles
Brand leadership + customer proof
Own ClinicMind’s review and reputation engine: customer advocacy motions, review generation campaigns, response governance, and proof rollups
Turn customer outcomes into trust assets that drive conversion (reviews, case studies, before/after workflows), aligned to vertical campaigns
Ensure third-party proof, such as G2, is consistently developed and used across campaigns, landing pages, and sales enablement
Partner with Customer Success to run customer advocacy + referral motions and support expansion campaigns (reviews, case studies, referral asks, upgrade nudges).
PatientHub-first marketing and sales operating model
Operate marketing workflows using PatientHub as the default system (campaign execution, follow-up workflows, reporting visibility)
Reduce reliance on disconnected tool sprawl and ensure internal usage becomes external proof (“we run our business on it”)
Build “how we use PatientHub” materials (SOPs, screenshots, short videos, templates) that Sales and Customer teams can use with prospects/clients
Team Leadership & Operational Scale
This is a founding leadership role. Early on, success comes from orchestrating a lean internal pod + agencies/contractors (creative, paid media, SEO, web, email ops, event production, etc.) with strong briefs, clear KPIs, and tight iteration cycles. Over time, you will help define which functions should be brought in-house and hire accordingly.
You will:
Lead cross-functional execution across Growth/Marketing, Agency, Events, Affiliates, and Sales enablement
Translate frontline sales feedback into improved targeting, messaging, and materials
Set standards for campaign briefs, launch QA, and performance reviews
Hold vendors and internal contributors accountable to KPIs (delivery + outcomes)
Create clarity on “who owns what” across motions (paid, events, organic, lifecycle) and prevent lead leakage through consistent follow-up and SLA adherence
Run a weekly WBR (weekly business review) with Sales/SDRs: SQL quality, SLA compliance, leakage reasons, and next actions.
This role requires comfort in being both strategic and hands-on. You are expected to ship consistently—running weekly launches/iterations with clear owners, QA gates, and deadlines.
Required Qualifications
7–12+ years in B2B marketing with significant time in demand generation / growth marketing roles
Proven track record of delivering qualified pipeline / SQL outcomes (not just leads), including measurable improvements in conversion rates (MQL → SQL, SQL → Opportunity)
Experience owning and optimizing multi-channel programs (paid, landing pages/CRO, lifecycle/email, content/SEO, webinars/events)
Demonstrated ability to manage agencies/contractors with clear briefs, KPIs, weekly performance reviews, and fast iteration cycles
Strong analytical discipline: comfortable with dashboards, attribution, funnel reporting, and budgeting tied to revenue outcomes
Able to operate as a player-coach in a founding environment—hands-on early, building process, and leverage through vendors before scaling headcount
Excellent cross-functional communicator with experience partnering closely with Sales/SDRs on lead definitions, routing/scoring, SLAs, and feedback loops
Able to quickly master and communicate ClinicMind’s value proposition (EHR + RCM + patient engagement, and the ‘compounding’ operating model) in a way that converts.
Experience building and maintaining third-party trust signals and customer advocacy (e.g., G2), turning proof into conversion
Comfortable dogfooding PatientHub: running marketing ops inside PatientHub and translating internal usage into customer-facing proof.
Demonstrated, hands-on use of AI to accelerate research, campaign development, creative iteration, and performance analysis (with strong judgment and QA).
Strongly Preferred Experience
Experience in marketing to SMB healthcare providers or practice leadership
Experience supporting multi-product or services-enabled SaaS platforms
Familiarity with demand generation, lifecycle marketing, and sales enablement
Experience working closely with Sales in a pipeline-driven organization
Comfort operating in fast-growing, execution-focused environments
Why Join ClinicMind
Work on a mission-critical healthcare platform with real operational impact
Clear scope, expectations, and accountability
Strong leadership and alignment with Growth and Sales
Opportunity to lead, build, and scale meaningful marketing programs
A clear path for growth as the organization scales
Must Have
Must have stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be comfortable working the US business hours (EST)
Must own a PC or laptop with at least 16 GB of memory
About ClinicMind
About the Role
We’re looking for a hands-on entrepreneurial leader to launch our Client Agency Partner Program — a model that turns our most successful clients into certified growth partners who scale their impact across other clinics.
This role sits at the intersection of Customer Success, Partner Enablement, and Growth Strategy. You’ll own the strategy that converts client outcomes into monetizable opportunities, expanding ClinicMind’s ARR and brand credibility through real success stories.
What You’ll Do
Client-to-Partner Growth
Identify top-performing ClinicMind clients and invite them into the Agency Partner Program.
Build scalable partner onboarding and enablement systems: certification, templates, marketing kits, and go-to-market support.
Develop monetization models (licensing, revenue share, managed services, partner bonuses).
Oversee partner governance, performance tracking, and delivery quality.
Scale the ecosystem to grow recurring revenue through client-led expansion.
Customer Success & Social Proof
Lead G2, Capterra, and review-driven growth campaigns to boost market visibility.
Launch Customer Success Celebration initiatives
Convert outcomes into verified reviews and success stories.
What We’re Looking For
5+ years in Customer Success, Partner Management, or SaaS Growth (GoHighLevel experience a plus).
Experience building scalable partner programs or ecosystem revenue models.
Excellent relationship management, communication, and operational design skills.
Entrepreneurial mindset with a proven ability to build systems from the ground up.
Key KPIs:
ARR from partner channels
#1 Ratings on G2 and Capterra in all the relevant ClinicMind Platform categories
Must Have
Must have stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be comfortable working the US business hours (EST)
Must own a PC or laptop with at least 16 GB of memory
Why Join ClinicMind
You’ll be building one of the most transformative growth engines in healthcare tech — where client outcomes become the foundation of expansion. If you’re energized by building, scaling, and celebrating success stories that drive real impact, we want to hear from you.
Apply now and help shape the next chapter of ClinicMind’s growth.
As a Senior GoHighLevel Developer, you will lead the design, development, and optimization of automation and integration workflows within ClinicMind’s environment. A critical part of this role involves implementing robust tracking and reporting mechanisms to measure the effectiveness of all GHL-driven initiatives. You’ll customize GHL to meet healthcare-specific needs, connect it with internal systems and third-party platforms, and ensure all automations are efficient, scalable, and HIPAA-compliant.
This is a highly collaborative, hands-on role ideal for a developer passionate about technology, automation, and data-driven optimization. You’ll work with teams across engineering, product, marketing, and operations to enhance automation reliability, provide actionable performance insights, and optimize patient journeys and business workflows.
Key Responsibilities
Architect, design, and implement advanced workflows, pipelines, and triggers within GoHighLevel.
Customize funnels, forms, scheduling systems, and automated communication sequences for patient engagement.
Integrate GHL with ClinicMind’s EHR, billing, CRM, and marketing systems via APIs and webhooks.
Develop and maintain custom scripts, functions, and automation logic for secure data handling.
Design, implement, and maintain custom reporting structures, dashboards, and analytics within GoHighLevel to provide key performance indicators (KPIs) on patient engagement, funnel conversion, and communication efficacy.
Troubleshoot and optimize automations for reliability, deliverability, and scalability.
Ensure compliance with HIPAA and healthcare data privacy regulations.
Document all workflows, integration logic, and best practices.
Collaborate with cross-functional teams to translate business needs into automation solutions.
Develop and execute data synchronization strategies between GHL, our EHR/CRM systems, and BI tools to ensure a single, accurate source of truth for all automation and patient data.
Mentor and support junior developers or automation specialists on GHL best practices.
Required Qualifications
5+ years of hands-on experience in automation development in GoHighLevel (GHL), including deep expertise in GHL’s reporting features, custom values, and data aggregation for performance measurement.
Proven experience with API integrations (REST, JSON, Webhooks).
Proficiency in JavaScript, HTML, and CSS for front-end customization.
Hands-on experience with Twilio, Mailgun, and other communication APIs (SMS, email, voice).
Familiarity with Zapier, Make (Integromat), Pabbly, or similar middleware tools.
Strong problem-solving, debugging, and documentation skills.
Excellent collaboration and communication skills in a remote, cross-functional environment.
Solid understanding of healthcare workflows, data handling, and patient engagement principles.
Qualifications
Experience in healthcare IT, EHR, or medical billing systems.
Knowledge of HIPAA compliance and data security standards.
Experience with white-label or multi-account GHL setups.
Exposure to serverless automation tools (AWS Lambda, Google Cloud Functions).
Familiarity with database integrations (MySQL, Firebase, Airtable, etc.).
Prior experience in agency or marketing tech environments.
Position Requirements
Must have a stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be in a quiet environment / work from home set-up
Must be comfortable working the US Eastern Time business hours
Minimum system requirement: Latest i5 with SSD hard disk (i7 preferred), 16GB RAM (32 GB preferred)
ClinicMind is a leading healthcare SaaS platform that helps outpatient practices improve financial performance, drive sustainable growth, and deliver better patient care. We bring EHR, revenue cycle management (RCM), patient engagement (PatientHub), credentialing, and payments together under one roof, with a strong focus on chiropractic, behavioral health, and physical therapy.
The Role
We’re looking for a hands-on Sales Manager to lead our new-business sales team (AEs + SDRs) and turn a proven go-to-market approach into consistent, predictable results. You’ll report to the CRO and own the day-to-day: coaching reps, running the sales rhythm, enforcing our playbook, and improving conversion rates across the funnel.
What You’ll Do
Lead, coach, and develop a small team of AEs and SDRs focused on new logo acquisition
Run daily/weekly training, call reviews, objection handling, and proposal reviews
Own execution of our sales playbook, pitchbook, and SOPs
Manage pipeline, forecasts, and CRM hygiene; run regular pipeline/deal reviews
Improve conversion at key stages (lead → opp, demo → proposal, proposal → close)
Partner with Marketing and our Affiliate Manager to maximize inbound and affiliate-sourced pipeline
Participate in hiring, onboarding, and performance management of reps
What Success Looks Like
Team consistently hits/exceeds new ARR quota
Higher conversion rates and a cleaner, more predictable pipeline
Faster sales cycles without discounting our value
New reps ramp quickly and reliably
What We’re Looking For
5+ years B2B sales, including 2+ years leading AEs and/or SDRs
Track record of leading a small team to hit/exceed quota
Strong coaching skills and comfort being deep in deals and data
Experience in enforcing a structured sales process and using CRM/metrics to manage
Experience selling into medical practices or healthcare tech
Location & Compensation
Work from Home, USA
Competitive base + variable (OTE) and benefits
Must Have
Must have stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be comfortable working the US business hours (EST)
Must own a PC or laptop with at least 16 GB of memory
About the Role
ClinicMind is seeking for a Content Specialist to create high-quality, strategic content that fuels our lead generation engine and strengthens ClinicMind’s position as the all-in-one platform for growing healthcare practices.
You’ll own the creation of marketing assets — from white papers and guides to workshops and videos — designed to attract, educate, and convert healthcare providers evaluating ClinicMind’s solutions. This role combines creativity, strategy, and performance-driven thinking.
Why Join ClinicMind
ClinicMind is a leading healthcare SaaS platform that helps providers improve their practice financial performance, drive sustainable growth, and enhance patient care with integrated EHR, RCM, and Patient Engagement automation and excellent service solutions.
Key Responsibilities
Develop value-driven content (white papers, guides, downloads) to support inbound and nurture campaigns.
Design and manage self-guided workshops and educational resources that help prospects and customers engage with ClinicMind’s platform.
Collaborate on video content such as explainers, case studies, webinars, and product walkthroughs.
Ensure all materials reflect ClinicMind’s brand voice— credible, insightful, and mentor-like.
Partner with product, sales, and marketing teams to identify content gaps and align messaging with business goals.
Stay informed on product updates and new features, developing subject-matter expertise to communicate them clearly and effectively.
Track performance and continuously optimize content for lead generation and conversion.
Requirements
3+ years of experience in content marketing or demand generation, preferably in SaaS or healthcare tech.
Proven track record creating high-performing content that drives measurable pipeline or lead outcomes.
Must share a portfolio of marketing assets created, along with examples of how each was used to generate leads or deliver measurable results.
Exceptional writing, editing, and storytelling skills across multiple formats and channels.
Comfortable collaborating with SMEs, designers, and video editors.
Must be able to overlap with U.S. working hours.
Bonus Points
Experience in healthcare, EHR, or medical billing software.
Familiarity with AI-assisted writing and marketing automation tools.
Experience running or supporting campaigns through HubSpot, Marketo, or similar platforms.
Must Have
1. Must have stable internet connection minimum of 25 MBP
2. Must have a mobile data plan as a backup.
3. Must be comfortable working the US business hours (EST)
4. Must own a PC or laptop with at least 16 GB of memory
Role Overview
ClinicMind is seeking a Social Media Coordinator to execute and manage our social media presence across priority platforms, with a strong emphasis on brand authority, demand generation support, and engagement with healthcare decision-makers.
This is a highly execution-oriented role that directly supports ClinicMind’s growth engine by amplifying campaigns, events, thought leadership, customer success stories, and product messaging. The ideal candidate understands how social media contributes to pipeline outcomes (MQLs, SQLs)—not vanity metrics—and can operate effectively within structured workflows, calendars, and performance expectations.
Key Responsibilities
Social Media Execution & Management
Manage day-to-day posting and scheduling across priority platforms, including:
LinkedIn (primary B2B channel)
X (Twitter), as applicable
Execute weekly and monthly social media calendars aligned with:
Demand generation campaigns
Events and sponsorships
Product launches and feature updates
Executive and thought leadership content
Ensure consistent brand voice, tone, and messaging aligned with ClinicMind’s positioning: “One Platform. One Growth Engine.”
Content Amplification & Cross-Functional Collaboration
Repurpose approved content into social-first formats, including:
Blogs and articles
Webinars and podcasts
Case studies and customer success stories
Events, press releases, and product announcements
Support amplification of:
Executive thought leadership (CEO, CGSO, product and clinical leaders)
Partner and affiliate content
Client wins, testimonials, and company milestones
Collaborate closely with:
Content Marketing
Events and Partnerships/Affiliates
Sales (for visibility, enablement, and alignment with pipeline priorities)
Engagement & Community Management
Monitor comments, messages, and engagement across platforms; respond directly or route appropriately
Actively engage with:
Industry leaders and influencers
Partners and affiliates
Clients and prospects
Event organizers and sponsors
Proactively identify opportunities for tagging, cross-promotion, and increased visibility
Performance Tracking & Optimization
Track and report on key social media KPIs, including:
Engagement rate
Follower growth (quality and relevance over volume)
Traffic to website and campaign landing pages
Campaign- and event-specific performance
Support marketing attribution by applying proper UTM tagging in coordination with Marketing Operations
Provide insights on content formats, topics, and channels that drive the strongest engagement and downstream impact
Required Qualifications
2+ years of experience managing social media for B2B companies (required)
Experience in healthcare, SaaS, or professional services environments (strongly preferred)
Strong understanding of LinkedIn as a B2B growth and thought leadership channel
Experience using social media scheduling and management tools (e.g., GoHighLevel or similar)
Excellent written communication skills with strong attention to tone, clarity, and brand alignment
Ability to execute within structured workflows, calendars, and deadlines
Advanced Canva editing and design skills
Preferred Qualifications
Experience supporting demand generation or revenue-focused marketing teams
Familiarity with healthcare, behavioral health, chiropractic, or practice management audiences
Experience promoting events and executing post-event amplification strategies
Basic understanding of UTM tracking and marketing attribution
Comfort operating in fast-paced, scaling organizations
What Success Looks Like in This Role
Social media clearly supports—and does not distract from—pipeline and revenue goals
Consistent, on-brand execution with minimal rework
Strong engagement from the right audience (owners, executives, decision-makers)
Reliable posting cadence aligned with campaigns, events, and launches
Clear reporting and actionable insights that inform future content and campaign strategy
Why Join ClinicMind
ClinicMind is a growing healthcare technology company modernizing how practices operate, grow, and scale. You will join a team that values clarity, accountability, and measurable impact, with the opportunity to contribute directly to brand growth, demand generation, and revenue-driving initiatives.
We are a Health IT and RCM service company with a leading-edge EHR software product and a medical billing BPO. We are looking for an enthusiastic Account Executive. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
The Account Executive will be responsible for identifying, nurturing, and closing new business opportunities within the healthcare space. You will work closely with marketing, product, and customer success teams.
Responsibilities:
Own the full sales cycle: prospecting, qualification, product demos, proposal development, and contract negotiation.
Develop and maintain strong relationships with key stakeholders in hospitals, clinics, and healthcare organizations.
Understand client needs and effectively communicate how our technology addresses pain points and delivers ROI.
Maintain a robust pipeline using CRM tools
Achieve and exceed monthly and quarterly sales targets.
Collaborate with Marketing to refine messaging and generate qualified leads.
Provide feedback to Product and Customer Success to align offerings with market demand.
Stay current on industry trends, regulatory changes, and competitive landscape.
Requirements:
2–5 years of experience in B2B SaaS sales, preferably in healthcare or health IT.
Proven track record of meeting or exceeding sales quotas.
Strong understanding of the healthcare market (providers, payers, EHR systems, RCM)
Excellent communication, negotiation, and presentation skills.
Self-motivated with strong time management and organizational abilities.
Proficiency in CRM and sales engagement tools.
Experience selling to healthcare providers, RCM teams, or hospital systems is an advantage.
Knowledge of HIPAA compliance, EHR systems, or healthcare billing workflows is an advantage.
Position Requirements
Must have stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be comfortable working the US business hours (EST)
Must own a PC or laptop with at least 16 GB of memory
We are a Health IT and RCM service company with a leading-edge EHR software product and a medical billing BPO. We are looking for an enthusiastic Sales Development Representative. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
Responsibilities:
Demonstrate basic functionality of our product.
Identify potential clients and generate new business opportunities for the company
Cold call potential clients to generate interest in our products and services
Send out personalized emails and LinkedIn messages to potential clients to nurture leads
Monitor appropriate social media groups/communities for potential leads
Schedule appointments with potential clients for the sales team
Provide accurate and up-to-date information on our products and services to potential clients, and this includes product and service demonstrations using presentation materials
Work with the sales team to develop strategies for lead generation and follow-up
Track progress towards meeting sales goals
Collaborate with the sales team to develop strategies for reaching sales targets
Use customer relationship management (CRM) software to manage leads and sales activities
Stay up-to-date on market trends, competition, and industry developments
Provide regular reports on sales activities and results to management.
Qualifications:
2-3 years of experience in sales.
Bachelor’s degree in business or related field
Experience in the healthcare industry preferred but not required
Excellent verbal and written communication skills
Ability to work in a fast-paced environment and handle multiple priorities
Strong interpersonal skills and ability to build relationships with potential clients
Self-motivated and goal-oriented
Proficient in Microsoft Office and CRM software
Position Requirements
Must have stable internet connection minimum of 5 MBPS
Must have a mobile data plan as a backup
Must be in a quiet environment
Must be comfortable working the US business hours
Must own a PC with at least 8 GB of memory
ClinicMind is a leading healthcare SaaS platform that helps providers improve their practice financial performance, drive sustainable growth, and enhance patient care with integrated EHR, RCM, and Patient Engagement automation and excellent service solutions. outcomes, and maximizes revenue cycle efficiency.
Position Summary:
The Junior Data Scientist will support the Data Science team in analyzing data, creating visual insights, and maintaining scalable data workflows using Amazon QuickSight and Amazon Redshift. This role is ideal for an entry-level candidate passionate about analytics, cloud data tools, and supporting data-driven business decisions.
Key Responsibilities
Data Management & Preparation
Extract, clean, and manage datasets within Amazon Redshift and related AWS data sources.
Ensure data quality, consistency, and completeness for downstream analytics.
Visualization & Reporting
Build and maintain Amazon QuickSight dashboards to communicate trends, KPIs, and actionable insights.
Automate recurring reporting workflows and enhance dashboard interactivity.
Data Analysis & Insights
Conduct exploratory data analysis (EDA) to uncover trends and patterns.
Support business teams by generating ad-hoc analyses and presenting insights clearly.
Collaboration & Support
Work closely with the Data Science Team Lead and cross-functional teams (Operations, Product, and Engineering).
Participate in sprint reviews, data validation, and stakeholder discussions.
Continuous Learning & Innovation
Stay up to date on AWS analytics services, BI tools, and data visualization best practices.
Contribute new ideas for improving efficiency, visualization design, and automation.
Skills and Qualifications
• Bachelor’s degree in Computer Science, Statistics, Mathematics, Data Analytics, or related field.
• Hands-on experience with Amazon QuickSight for dashboarding and reporting.
• Understanding of Amazon Redshift (queries, schemas, joins, and data pipelines).
• Knowledge of SQL for data extraction and transformation.
• Basic exposure to Python or R (optional but desirable).
• Strong analytical mindset and attention to detail.
• Good communication and presentation skills.
Preferred Certifications
• AWS Certified Data Analytics
• Amazon QuickSight Author Certification
• AWS Cloud Practitioner or Practitioner Essentials
Must Have
ClinicMind is a leading healthcare SaaS platform that helps providers improve their practice financial performance, drive sustainable growth, and enhance patient care with integrated EHR, RCM, and Patient Engagement automation and excellent service solutions.
Role Overview
The Sales Executive – Growth & Events is a quota-carrying role responsible for driving new business and expanding existing accounts through both event-based and self-generated sales activity.
You’ll manage the full sales cycle from discovery to close, represent ClinicMind at national events, and proactively build your own pipeline between shows.
This position is for a closer who thrives in fast-paced environments, loves consultative selling, and is comfortable being measured by results, not effort.
Key Responsibilities
New Business Development
Prospect, qualify, and close new accounts in behavioral health, chiropractic, and multi-specialty verticals.
Run full-cycle sales: discovery → demo → ROI presentation → proposal → close.
Use ClinicMind’s ROI Calculator and DPA framework to quantify value and build business cases.
Maintain a healthy 3x quota pipeline in CRM, reporting weekly progress to the CRO.
Event Sales & Representation
Represent ClinicMind at trade shows, partner events, and conferences.
Pre-book at least 10 qualified meetings per event and generate a minimum of 30 new SQLs.
Close deals directly at events when possible and follow up on all contacts within 48 hours.
Collaborate with Marketing to measure event ROI and improve future event strategies.
Self-Sourced Pipeline
Generate new opportunities between events through outbound prospecting, networking, and follow-ups.
Maintain a consistent self-generated pipeline covering 3x monthly quota.
Use LinkedIn, referrals, associations, and regional partnerships to identify new targets.
Account Expansion
Identify cross-sell and upsell opportunities within existing accounts.
Partner with Customer Success to identify expansion opportunities post-implementation.
Performance & Reporting
Meet or exceed assigned new ARR and upgrade quotas.
Maintain CRM hygiene (≥90% data completeness).
Report weekly on pipeline health, conversion rates, and event ROI.
Qualifications
3–6 years B2B SaaS or healthcare tech sales experience.
Proven quota attainment and strong closing track record.
Consultative selling skills; comfortable using ROI tools and financial modeling.
Excellent communication, presentation, and relationship management.
Entrepreneurial, self-motivated, and able to work independently.
Comfortable with 30–40% travel.
KPIs
Monthly new ARR closed
Event pipeline generated & SQL-to-close ratio
ROI Calculator usage rate
Demo-to-close conversion %
CRM data accuracy (≥90%)
Post-event follow-up within 48h
Must Have:
Must have stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be comfortable working the US business hours (EST)
Must own a PC or laptop with at least 16 GB of memory
Why Join ClinicMind
You’ll represent one of healthcare’s fastest-growing technology platforms and see direct, measurable impact from your work.
We give you the tools, autonomy, and support to build your own book of business, while aligning with a team that wins through collaboration, accountability, and clear ROI outcomes.
ClinicMind’s core values—Excellence · Learning · Teamwork guide everything we build.
With 150 in‑house analysts, half a dozen BPO partners, and a proprietary billing platform, we now need a manager to deliver best‑in‑class collections, continue to improve performance, automate, and meet the RCM needs of a rapidly growing client base.
Overview
We are seeking a Level 3 Billing Support / Billing Review Subject Matter Expert (SME) to join our team. This role serves as the final point of escalation for complex billing concerns and systemic claim issues. The SME team ensures accuracy in claim processing, resolves systemic billing setup problems, and provides expert support to billing staff, providers, and retention teams. Experience with ClinicMind/Vericle software is required.
Key Responsibilities
Handle high-level billing escalations and serve as a subject matter expert for complex claim issues.
Review claims to identify errors caused by system setup or process gaps.
Collaborate with SYSADMIN to correct systemic configuration issues and validate updates.
Provide data and guidance on affected claims to billing teams and providers for manual resolution.
Support provider and retention teams by explaining billing outcomes and corrective actions clearly.
Document recurring issues and recommend workflow or system improvements.
Mentor Level 1 and Level 2 billing support staff, sharing expertise and best practices.
Lead or participate in small projects related to billing reviews, system changes, and process enhancements.
Qualifications
Bachelor’s degree in Business, Healthcare Administration, Finance, or equivalent work experience.
4–6 years of experience in medical billing, claim review, or revenue cycle management.
Mandatory: Hands-on experience with ClinicMind/Vericle software.
Strong knowledge of billing workflows, claim adjudication, and payer requirements.
Excellent communication skills to interact with providers, billing teams, and technical staff.
Strong analytical and problem-solving abilities with attention to detail.
Basic project management experience (managing timelines, priorities, and stakeholder coordination).
Preferred Skills
Prior experience collaborating with system administrators on billing setups.
Knowledge of compliance standards and payer regulations.
Ability to train or mentor junior staff.
Must Have:
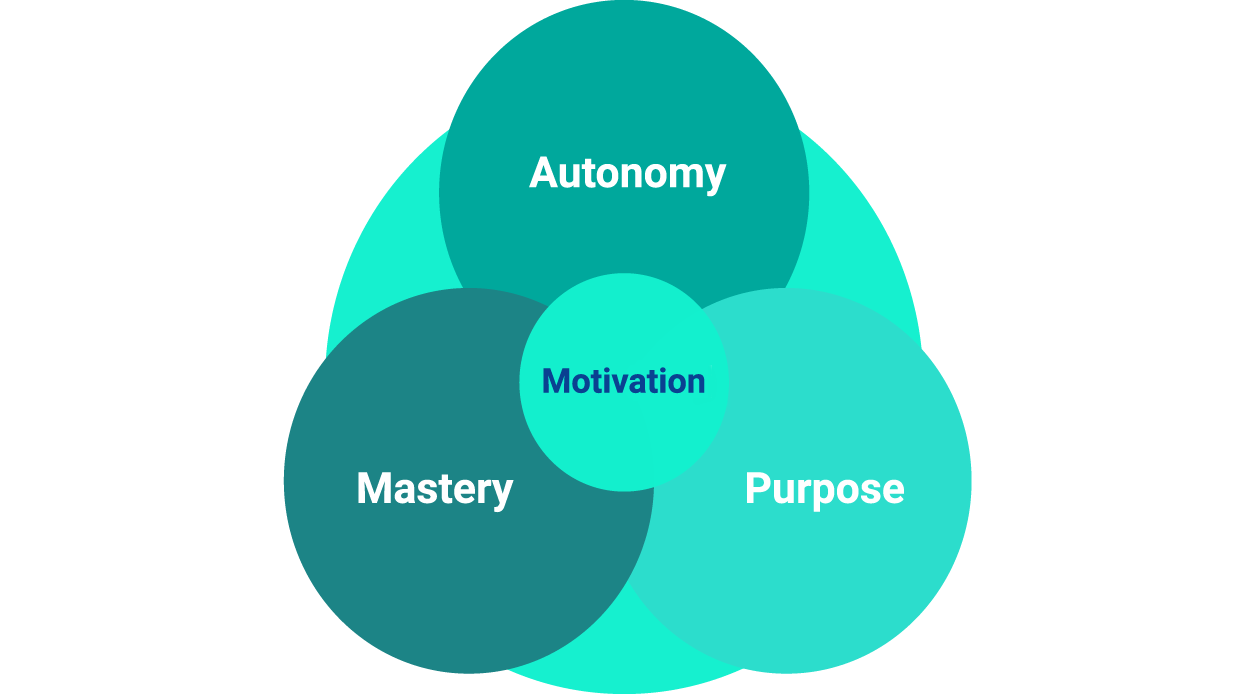
We strive for excellence throughout our hiring process.
We share the purpose of making a lasting change in the healthcare industry by building together state-of-the-art software and using it to level the playing field with the payers.
We invest our energies in learning and mastering our skills, and we grow our responsibilities in step with our professional and business growth.
This site includes cumulative user rating numbers, video testimonials, press releases, and other social proof materials across all brands and all resellers leveraging ClinicMind Software and/or Service as a Platform (SaaP). For more detail about our white labeling and reselling models, visit our About Page or Contact Us directly. Check Privacy Policy