ClinicMind 2.0 Mobile EHR: Now Available on iPad
ClinicMind 2.0 is now available on iPad, bringing full mobility to your electronic health records (EHR). With ClinicMind’s Mobile EHR, providers can securely access patient charts, billing, and scheduling from anywhere. This next-generation update delivers faster documentation, streamlined workflows, and a seamless experience across desktop and mobile. What’s New with ClinicMind 2.0 on iPad: ClinicMind 2.0 Doc & Bill on iPad – Access the redesigned patient chart, billing, scheduling, and more with the same intuitive workflows you already know. Streamlined Interface – Enjoy a modern, simplified design that helps you chart faster, reduce clicks, and focus more on patient care. Full Integration on the Go – From intake to documentation to billing, everything works seamlessly across desktop and mobile, giving you true flexibility. Why Mobile EHR Access Matters for Providers: ClinicMind 2.0 is one of our initiatives built to help practices reduce admin burden, increase compliance, and accelerate documentation. Now, with full iPad availability, providers gain: True mobility: Work securely from anywhere Smarter workflows: All-in-one access to scheduling, billing, and patient charts Future-ready EHR: Stay ahead with the system designed for long-term growth This update isn’t just another version, it’s a major milestone. The early release makes this upgrade available sooner than expected, underscoring our commitment to innovation. Get Started with ClinicMind Mobile EHR Today: Ready to experience ClinicMind 2.0 on your iPad? Update to Mobile EHR today and bring the future of healthcare documentation wherever you go.
Stop Losing Patients to Missed Calls: Why Chiropractors Need a Virtual Front Desk Solution
When a patient call goes unanswered, the cost isn’t just one appointment—it’s lost revenue, patient frustration, and a damaged reputation. For many chiropractic practices, missed calls and scheduling gaps are silent profit killers. Front desk staff already juggle a mountain of tasks: greeting patients, verifying records, handling billing questions, and managing walk-ins. Adding nonstop phone coverage on top of that almost guarantees missed opportunities. That’s where ClinicMind’s Virtual Front Desk (VFD) comes in. From Overloaded Chiropractic Staff to a Virtual Front Desk Solution Too often, practices rely on voicemail, overworked staff, or generic reminder systems. The result? Missed appointments, delayed callbacks, and patients slipping through the cracks. ClinicMind’s VFD is different. It’s not just a reminder tool—it’s a fully integrated call answering and scheduling support service designed for healthcare practices. Think of it as your outsourced front desk team, trained on your workflows, running reliably behind the scenes. How ClinicMind’s Virtual Front Desk (VFD) Works The Virtual Front Desk keeps your schedule full and your patients supported, without burning out your staff. Core Features: Live call handling, Mon–Fri, 8 AM–8 PM EST Voicemail fallback after hours (with a guaranteed 2-business-hour callback window) Real-time scheduling directly inside ClinicMind’s EHR Custom scripts & FAQs tailored to your practice HIPAA-compliant communication through ClinicMind Task Workbench Call tracking & 1-year recording storage for quality and accountability Services Provided: Appointment booking, rescheduling, and cancellations Overflow call handling when your staff is busy Patient intake and general inquiries Collecting and forwarding messages Voicemail callbacks Why Chiropractors Choose ClinicMind’s Virtual Front Desk Over Call Centers Unlike generic call centers, ClinicMind’s Virtual Front Desk was built for healthcare practices already using ClinicMind. That means: Cost Efficiency: $300/month for 300 minutes—far more affordable per minute than Ruby Receptionists, AnswerConnect, or Smith.ai. Seamless EHR Integration: Schedule management directly inside ClinicMind’s system, no third-party tools required. HIPAA Compliance: Secure communication that protects patient data—something competitors don’t always guarantee. Custom Call Scripts: Every call handled your way, reflecting your practice’s voice and priorities. Faster Follow-Up: 2-hour voicemail callback SLA, reducing patient frustration. Benefits of a Virtual Front Desk for Chiropractors With VFD, chiropractors eliminate the top scheduling and communication challenges that drain time and revenue: No more missed patient calls → capture every opportunity. No more double-bookings or gaps → maximize provider time. No more burned-out staff → let your team focus on in-office care. The outcome? Higher patient satisfaction, stronger retention, and a predictable schedule that drives growth. Get Started With ClinicMind’s Virtual Front Desk Don’t let unanswered calls cost your practice revenue. ClinicMind’s Virtual Front Desk is the smarter, HIPAA-compliant way to keep your phones covered and your schedule full—without adding headcount. Book your free consultation today and see how VFD can help your practice acquire and retain more patients.
PatientHub Scheduled Maintenance Notification
We want to inform you about upcoming scheduled maintenance to ensure the continued reliability and performance of PatientHub. Maintenance Details: Dates: January 17–19, 2025 Start Time: 4 PM ET Expected Duration: 48 hours During this time, PatientHub will continue to function normally. However, any new patients or appointments will not sync to PatientHub. Once the sync is restarted, PatientHub will catch up and the sync will continue normally with no intervention needed. We apologize for any inconvenience this may cause and thank you for your understanding as we work to enhance our services.
Computer-aided Patient Scheduling
Without a computerized scheduler, a practice has less than a 2% chance of earning the title of a “better-performing practice,” according to the Medical Group Management Association. Computerized scheduling helps decrease service costs, provide fairness in service delivery, increase patient satisfaction, and reduce waiting times (Zhang et al., 2019). A massive investment in scheduling features across a wide spectrum of billing products indicates the importance of computerized scheduling. Convenience and front office efficiencies are two obvious benefits of a computerized scheduling system; without them, the only manual way to find out if a specific patient has a scheduled appointment is to flip through the appointment book page by page. Worse, manual scheduling hurts both patient satisfaction and practice financial performance because of scheduling inconsistencies and unbilled (and therefore unpaid) visits. But the benefits of integrated computerized scheduling stretch far beyond convenience, front office efficiencies, and better charge follow-up of stand-alone, albeit computerized, scheduling. A well-designed and integrated scheduler allows preferential patient scheduling, which, along with improved controls, helps revenue optimization and practice compliance. Next, we review key aspects of computerized scheduling and demonstrate the important benefits of integrated scheduling, billing, and compliance management. Scheduling Policies Computerized schedulers allow a combination of single- or multiple-interval scheduling, with open-access scheduling subject to various priority constraints. Such priority-constraint-driven, open-access scheduling creates preferential appointments based on patient demographics or insurance coverage. Typical time-slot-based appointment systems essentially divide a physician’s schedule into finite slots in a day, which can be allocated according to appointment requests. However, such systems are limited by the risks of schedule fragmentations in late shows or no-shows (Chen et al., 2019). Examples of time-slots-based scheduling include single-interval scheduling and multiple-interval scheduling. Single-interval scheduling allocates appointments at regular intervals of 5 to 15 minutes, depending on the specialty. The downside of single-interval scheduling is that as soon as one appointment takes longer than the allocated slot, all subsequent patients must wait. Multiple-interval scheduling also sets appointments at regular intervals; however, unlike single-interval scheduling, it allocates the appointment length depending on the chief complaint. Such scheduling requires up-front categorization of key appointment types and their projected lengths. For instance, an initial appointment might take 30 minutes, while a routine injection might take only 5 minutes. According to the CAHPS survey database, about 12% of patients who called in did not get appointments for urgent care that they needed at the time. Forjuo et al., (2001) also showed that inadequate access to primary care providers was a leading cause of patient dissatisfaction. These challenges are mitigated by open-access scheduling. Open-access scheduling requires holding several appointments open every day. These open appointments are filled only within 48 hours of the appointment, catering to same-day or last-minute patient requests. Open-access scheduling improves access to the physician, reduces no-shows, and eliminates patient screening time. The downside of open-access scheduling is, of course, the potential for longer patient waiting lines or physician idle time because of the inability to maintain a predictable patient flow. A novel scheduling variant is the overlapping appointment scheduling (OLAS) model (Huet et al., 2020). OLAS model refers to deciding the optimal overlapping periods between the patient appointment and allocated service times. The model is formulated as an optimization problem to minimize the total cost of patients waiting and doctors’ idle time. One way to balance the practice workload is to schedule group, routine, or repeat appointments during slow hours. For instance, pediatric well-child visits or patients with a particular chronic disease—such as congestive heart failure or diabetes—could be scheduled for early mornings when there are typically fewer patients waiting in line. These scheduled visits include educational components and often involve multidisciplinary teams. It also helps save time since standard advice need not be repeated to individuals, improving on the efficiency of care delivery (Jones et al., 2019). Patients also benefit from the socialization aspect of group visits; members encourage one another, exercise together, and so forth. A good scheduler allows a repeat appointment schedule subject to total frequency and time slot constraints. Compliance Process An integrated scheduler verifies the filing of a signed patient consent form—and, in certain cases, a signed ABN form. An ABN (Advance Beneficiary Notice) serves three goals: To protect the beneficiaries from liability for services denied as not reasonable (depends on the frequency or duration) and necessary (depends on the diagnosis and the provider’s specialty) To protect the provider’s revenue by shifting financial liability for denied services to the patient To provide documentation for a Medicare audit For more complex procedures, the scheduler warns the front office about the need to obtain all required diagnostic test results and clearances up front. Billing Interface The integrated scheduler avoids unbillable patient encounters and reconciles visits with patient balances. It checks outstanding patient balances and verifies coverage and eligibility at the point of scheduling before the appointment. AI-driven computerized coding and billing systems can accurately provide the code for a particular disease condition and help with appropriate automated billing (Venkatesh et al., 2023). In many cases, such a test discovers data entry errors too, reducing the payment cycle at later stages. Additionally, the insurance company may require referrals or separate pre-authorization/certification for certain procedures, refusing the payment if the procedure was performed without a referral or preauthorization. The integrated scheduler can access medical records to supply necessary background and diagnosis information to obtain pre-authorization. Finally, without the ability to reconcile visits with payments, the practice owner cannot be sure that every visit resulted in a payment. Practice Flow Interface The integrated scheduler manages the entire patient flow, continuously updating arrival lists, checkoffs, and office/room tracking. Further, the scheduler tracks no-shows and follow-up actions. Detailed reports include daily schedules, load reports, missed appointments, free time, canceled appointments, etc. With AI-integrated schedulers, different color codes and status flags can be used for different appointment types, whether emergencies or routine or based on the specialist to be seen by the patient. This offers a good visually appealing summary by just glancing over the
Customizable 2nd Appointment Schedule Alert Pop-ups
Introducing the Newest Feature of Genesis Chiropractic Software: Customizable 2nd Appointment Schedule Alert Pop-ups We are excited to announce the release of our latest feature in Genesis Chiropractic Software: customizable alert pop-ups. This new setting allows users to have more control over the alert pop-ups that appear on the schedule page when scheduling a patient for a second appointment. Previously, the pop-up would appear every time a patient was scheduled for a second appointment, regardless of the practitioner or schedule they were booked with. With our new optional setting, users can now choose to schedule the patient with a different practitioner or on a different schedule without the pop-up alert. However, if a second appointment is made on the same schedule, the pop-up alert will still appear. Users also have the option to turn off the pop-up alert altogether, allowing them to schedule patients for multiple appointments without being alerted each time. If you’re interested in changing how your pop-up alerts currently work, simply contact our training team, and they will update the setting for you. This new feature provides greater flexibility and customization options to our software, making it easier for chiropractors to manage their patient schedules and improve their overall workflow. We are thrilled to introduce this new feature and hope that it will enhance the user experience for our customers. Stay tuned for more updates and exciting features from Genesis Chiropractic Software.
Creating a Fee Schedule for Your Private Practice

Creating a profitable and fair fee schedule is crucial for private practices. It should cover true service costs, not just insurance reimbursement. Align your rates with insurance provider maximums and industry standards. Ensure consistency and notify patients in advance of any fee changes. Consider your practice’s operating expenses for an accurate fee structure. ClinicMind’s EHR/RCM platform simplifies fee schedule management and practice operations.
Chiropractic Office Owners Now Use Genesis Scheduling Workflow to Manage Patient Experience and Improve Compliance

Genesis Chiropractic Software by Billing Precision introduces Patient Appointment Workflow Management to help practice owners manage patient relationships (PRWEB) MAY 11, 2015 Genesis’ patient scheduling management simplifies patient appointment tracking and followup. Practice owners keep track of patient schedules and all relevant work in a single place. Learn about Genesis Chiropractic Software scheduling workflow to manage patient relationship here. According to Dr. Matthew McAlees, DC and owner of Charlotte Health Center practice, Genesis Chiropractic Software is what enables his staff to be both effective and efficient about patient relationship management. “Coming from a Family of Chiropractors, my Grandfather was a Chiropractor, my Father was a Chiropractor, and I’ve seen virtually every software program out there. The thing I love about Genesis is how easy it is and my staff loves it.” [/vc_column_text][vc_video link=”https://youtu.be/QdERc4mpFb4″][vc_column_text] According to Dr. Brian Capra, DC and President of Genesis Chiropractic Software, patient experience management is key for practice success. “Genesis Scheduling Workbench automates the process of patient scheduling and follow up and provides both the big scheduling picture and the fine resolution picture at the same time,” says Capra. “Genesis helps practice owners create a systematic patient relationship monitoring, control, and improvement process.” Patient experience management is key for practice success. – Dr. Brian Capra Learn about Genesis Chiropractic Software scheduling workflow to manage patient relationship here. About Genesis Chiropractic Software and Billing Precision, LLC Genesis Chiropractic Software by Billing Precision was designed by chiropractic business owners with both patient experience and practice profitability in mind. Genesis chiropractic software provides a complete chiropractic practice management system that supports every role in a busy chiropractic practice, from the owner and practitioners to the front desk and back office. It automates the vast majority of standard tasks, including patient relationship management, revenue cycle management, compliance and office management. Its exclusive workflow functionality continuously improves productivity, control and predictability, fostering teamwork and time savings, which leads to greater profitability and practice growth.
Three Ways To Schedule More Spinal Screenings In Your Community Today!

Dr. Tabor Smith has done over 300 spinal screenings so far in his career, and every month he adds 2-3 more screenings to that total. Today he runs a thriving practice in Houston TX that he built from the ground up, through consistent spinal screenings and monthly dinner workshops. Genesis Chiropractic Software recently connected with Dr. Tabor and asked him to share some strategies on how chiropractors can set up more screenings in their community. Below are 3 different ways to find more screening opportunities in your community. According to Dr. Tabor, the key to setting up screenings is to be persistent and consistent with your efforts. You may not be successful in your first few attempts, but that doesn’t mean you give up. It means you get excited because you are that much closer to success! 1. Know the schedule of every big venue in your community. This one tip can make a huge difference in your practice. If you want to grow your practice and get more involved in your community so you can help more people, then you need to be at every event that happens around your office. The best way to stay up-to-date on community events is to go to the place that big events happen. If you know the schedule of every civic center, gymnasium, and large auditorium in your community you will never miss the “next big event”! 2. Use Google to find shows and fairs going on in your community. You or your staff should be searching for events at least once a month. Schedule a time to sit down on your computer and search for events, shows, and fairs. Here is how you do it – First, go to Google.com, then type in “Events” and “Your Zip Code”. You will find page after page of listings. Go through each one and determine whether or not it would be a good fit for your office. Make a list of the events you want to attend so you can follow up later. Then go back to Google.com and type in “Show” and “Your Zip Code”. You will find page after page of listings. Go though each one and determine whether or not each show would be a good fit for your office. Make a list of the shows you want to attend so you can follow up later. Then go back to Google.com and type in “fair” and “Your Zip Code”. Again, you will find page after page of listings. Go through each one and determine whether or not it would be a good fit for your office. Pay particular attention to Health Fairs as they can be some of the best places to do a spinal screening. 3. Contact all the Corporations and businesses in your community, and ask them if they have an annual health fair. Granted, this is hit-or-miss, but you would be surprised at how many churches and corporations in your community actually have annual health fairs. You can use the same Google.com method described above to locate and gather contact info for all the corporations and churches around your office. Then call them and simply ask them if they have an annual health fair. If they do, ask them how you can get involved. If they don’t ask them if you can help them to start one! Thanks for taking the time to read my blog. If there’s ever anything I can do for you, let me know. Tabor Smith D.C.
Genesis Chiropractic Software and Custom Chiro Solutions Help Doctors Implement Compliant Fee Schedules

Custom Chiro Solutions and Genesis Chiropractic Software teaches Chiropractors how to maintain billing compliance for both insurance and cash patients. Custom Chiro Solutions and Genesis Chiropractic Software help chiropractors implement their billing methodology and compliance protocols on a consistent and controlled scale. “Maximized Living network helps take the pressure off me by helping me find the right chiropractic software, billing service, and compliance team. They help find the answers and implement them in all of our practices. We work as a team.” – Dr. Drew Kaminski, owner of Back On Track Family Chiropractic See Full Press Release Here: http://www.prweb.com/releases/2012/9/prweb9877225.htm Now a certified EHR/EMR! Powered by Vericle, Genesis Chiropractic Software, a product of Billing Precision, LLC, is a state of the art, web based “cloud” chiropractic software with an optional chiropractic billing service. Genesis uses the data that is stored in the cloud across hundreds of doctors. Unlike any other system that data is used to improve its built in artificial intelligence ability to automate workflow in relation to Patient Retention, Cash Flow, and Compliance. Genesis has the fastest compliant SOAP capability on the market, touch screens for all patient interactions, iPad ready and much much more.
Chiropractic Scheduling Solution – Billing Precision
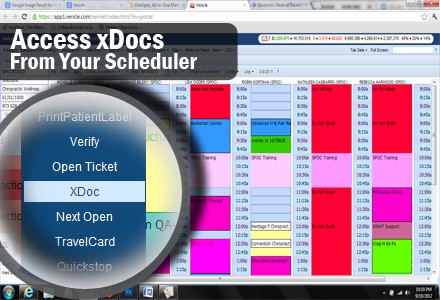
Scheduling: Billing Precision’s Chiropractic Billing Software provides every tool needed by your Chiropractic Office to succeed. One feature is the Schedule which many doctors have described as the best Chiropractic Scheduling Solution. The schedule features alerts,notifications and pop-up messages that remind you of anything related to the patient when the patient checks in. Billing Precision’s software product has been re-branded as Genesis Chiropractic Software. https://youtu.be/hBhHyBaS2Aw

