Documenting Subjective Complaints
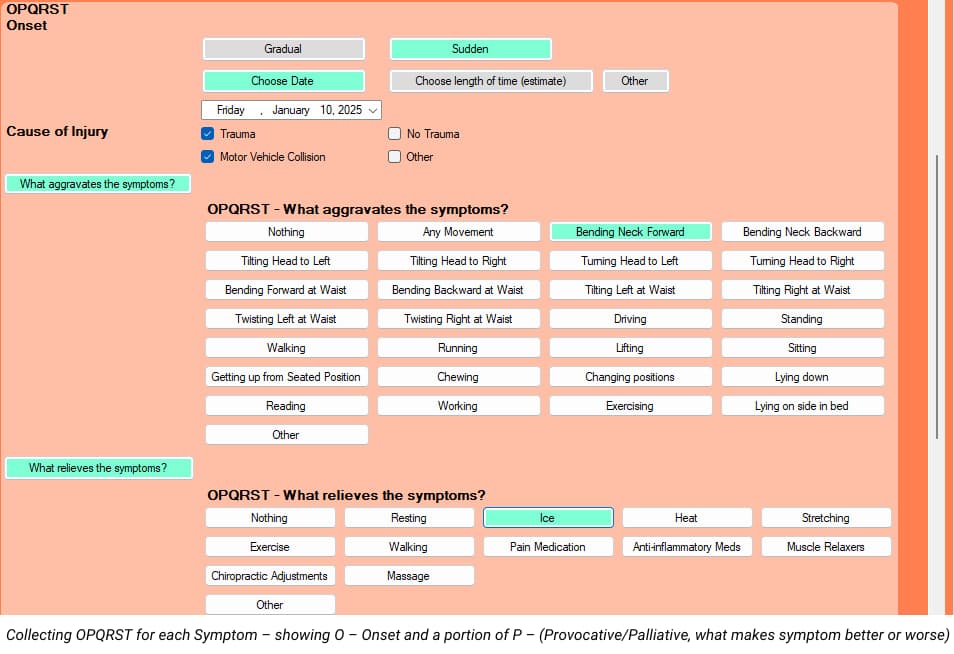
After being in practice for 32 years, teaching documentation and coding for about 20 years, reviewing records and performing IMEs for a lot of years, I see and hear the same things over and over again with regards to documenting subjective complaints. Let’s make this easy. Initial Visit According to the Mayo Clinic, 80% of the proper diagnosis comes from a good history. Unfortunately, many chiropractors tend to take shortcuts on the history, perhaps in the interest of saving time. The standard of history taking has been the OPQRST for many years. There are a few variations of this, but they all tend to get the same information. Before you think of not asking and documenting all of OPQRST, think about which of these items are less important than others. I teach doctors to document ALL of OPQRST on the first visit for ALL new patients, but there’s an easy and fast way to do it. Once we get that information at the beginning of a case, we don’t have to document all of that on subsequent visits. So, let’s review the OPQRST: Onset – when the patient presents with multiple conditions for which you will treat, you need to document OPQRST for EACH complaint, not just the CHIEF complaint. You’ll want to document how each condition started (trauma vs. no trauma), when each condition started (specific date or time frame) and if each symptom began suddenly or gradually. Provocative/Palliative – document both provocative and palliative for EACH condition you’ll be treating. In other words, what makes the neck pain better and worse, what makes the low back pain better and worse, etc. Quality – describe the quality of EACH symptom you’ll be treating. Radiate – document if each condition is radicular or not. If a symptom is radicular, use the language of Anatomical Position so anyone seeing your records will know what you’re talking about. For example, in the language of Anatomical Position, “arm” refers to above the elbow and “forearm” refers to below the elbow. “Thigh” refers to above the knee and “leg” refers to below the knee. You can be specific by documenting the neck pain radiates to the right posterolateral arm, right posterolateral forearm and to the first 2 digits of the right hand. Site/Severity – Be specific without going overboard. Instead of documenting “headaches”, we can document “occipital headaches.” For neck and back pain, we can document if it’s the whole neck or back or left or right. For severity, more and more payers and even reviewers like me want to see a 0-10 pain scale (10 being the worst pain imaginable) for each complaint. To make this easier for my patients, I start by asking them if they would call their pain, for each symptom, Mild, Moderate or Severe. If they say Mild, I explain that’s between a 1 and a 3 and ask them for a number. For Moderate, that’s between a 4 and a 7, and for severe, that’s between an 8 and a 10. That tends to make it easier for them to come up with a more accurate number. So, ask verbally for mild, moderate or severe for each symptom, but only to get them to an actual number that you’ll document. Timing – On the first visit only, document, for each symptom that you’re treating, if the pain is worse at a particular time or times of the day (morning, afternoon, evening, night), or if the symptom is unaffected by time of day. For all visits, document what percentage of their awake time they notice each symptom. BEWARE of using the ranges of Occasional, Intermittent, Frequent and Constant, though. These ranges are defined as: Occasional: 0-25% of awake time Intermittent: 26-50% of awake time Frequent: 51-75% of awake time Constant: 76-100% of awake time The problem with these ranges is that they’re too broad (25 points). Your patient’s symptom could appear stuck in a particular category for MONTHS, which can make your documentation weaker by showing no change. Instead, I recommend document an actual percentage of time that each symptom is noticed (5 or 10 percent increments, though-don’t get carried away by documenting “23% of the time.” If you document on one visit that the frequency of the symptom was 100%, but on the next visit it reduced to 95%, even though just a slight change, it’s still shows some improvement. It’s much better to show the frequency went from 100% to 95% to 90% to 85% to 80% to 75% than to show constant, constant, constant, etc. Gregg’s Tip: I designed my intake paperwork to capture all of this information, so my patients do all of the heavy lifting for me. We send them the paperwork via e-mail and instruct them to bring the completed forms with them to their appointment. I also designed my EMR to be the same flow and direction of my paperwork, which makes it MUCH easier for the doctor or staff to input the information. Once we get all of that information entered on the first visit, all subsequent visits are QUICK AND EASY – I just change the metrics of the Severity and Frequency of each symptom. The next part of documenting subjective complaints is to establish a “measurable baseline of function” for each complaint. A great, easy, fast and inexpensive way to do this is with valid and reliable outcome questionnaires. Medicare requires this, many commercial insurers require this and for workers comp and PI, us reviewers are looking for this. You want to document the scores on the outcome questionnaires on the very first visit, which can then be used as a treatment goal. While Medicare requires that we perform these functional outcome assessments at a MINIMUM of every 30 days, I recommend performing these outcome questionnaires every two weeks for the active patient and once or twice per year for maintenance patients. If all chiropractors would do these outcome questionnaires every 2 weeks for ALL active patients, our documentation would be tremendously improved overnight. Gregg Friedman, DC,
Just Two Things
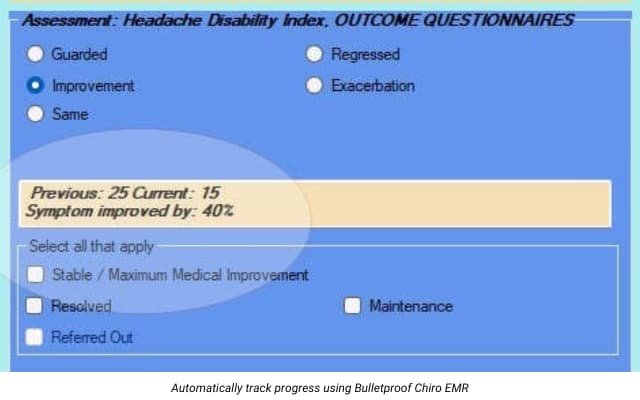
I remember the “good ‘ole days” of chiropractic. The days when it seemed that everyone in America had health insurance, when the typical deductible was about 100 bucks and the patient only had to pay 20% of the charges. And their policy limited chiropractic treatment to only “UNLIMITED VISITS.” Sigh… When a new patient came in, we did the ortho/neuro exam we all learned in chiropractic school, found a few areas of pain, some radicular signs every now and then and recommended a treatment plan. Patients seemed happy to start, excited it was affordable (since their insurance paid for the bulk of treatment). They started feeling better quickly and referred their friends and family in. And let’s not forget our favorite Medicare patients! Once they felt better, many of them wanted to continue to come in for maintenance. Yep, we just kept on billing Medicare…for years. For the personal injury patients, we’d examine, treat and bill, for pretty much as long as we wanted or until we got bored. No one ever challenged us. We’d send our bill in, and it got paid. All of it. Every penny. And no one ever asked to see our documentation. Ahhh…the good ‘ole days. That was about 30 years ago. I guess you can say it’s changed a bit since then. These days, patients may have health insurance, but their deductible is often higher than $5000 per year and co-pays are often more than our cash fee for an adjustment. Medicare is mad at us. Personal Injury is mad at us. Workers Comp, in many states, won’t even talk to us. Chiropractic offices are opening up all over the country, charging about $15 for an adjustment. Yeah, that helps. We were taught in chiropractic school and by every consultant on the planet to perform periodic re-exams on each patient. We’d find that the orthopedic tests caused a little less pain, palpation seemed to cause a little less tenderness and range of motion seemed to be getting better, as far we could tell. More and more, chiropractors are being asked to send our records to the insurance company so they can see if our treatment is appropriate. How rude. So, we send in a copy of our travel card, or even better, our fancy type-written notes from some EMR or EHR that we spent way too much money on or took more time to document than it did to adjust the patient. We send in our exam forms that show the patient is feeling less pain, less tenderness and seems to be moving better. And then we get told that our care was not “medically necessary” and no more treatment is appropriate. What in the world are they talking about? I know many doctors reading this are nodding their head in agreement. I got upset over the way I felt I was being treated, so I made it my mission to find out what the heck they were talking about. Apparently, someone changed the rules of documentation and no one bothered to tell us about it. So, what did I discover? The health care industry (doctors, insurance people, even attorneys) love tests. More specifically, tests with numbers. Think about it – blood tests have numbers. Urinalysis tests have numbers. All kinds of tests have numbers. What does a typical report of findings sound like from a medical doctor? Think about it. “Well, Mrs. Smith, we had some blood work done for you, and this is what we found. This is normal. This is you.” The patient nods. The doctor explains what it means and recommends some medication that the patient should take three times per day for the next 6 weeks. The patient nods. The doctor continues that, in six weeks, we’ll re-do the blood tests and see if the patient is normal or, at least, on the right track or not. The patient nods. Hopefully, as the tests become normal, the patient feels better, too. There was no selling involved. Just a doctor being, well, a doctor. So what are we chiropractors supposed to do? I mean, it would be AWESOME if we had a blood test that shows that the patients have subluxations here, here and there. It would be FANTASTIC if we could test their blood again after we’ve treated them for a period of time and see that their subluxations are improving here, here and there. Maybe one day we’ll have those kinds of tests, but for now… We don’t need them. The health care world basically wants two things from chiropractors. They want us to show that we have relieved the patient’s pain and improved their function. That’s it. Pain and function. Medicare now requires ALL doctors to report certain measurements to them to show that the treatment is being effective. Luckily for chiropractors, they currently only require TWO things. That’s right – Pain and Function. As a reviewer for many personal injury cases, I can tell you we look for the same two things – Pain and Function. What do the Workers Comp carriers want? Yep – pain and function. Think about your cash paying patients. Sure, they love it that they’re feeling better, but don’t you get excited for them when they say that they were able to play on the floor with their kids for 10 minutes longer than they could before? Or they’re driving a golf ball 30 yards farther than they did a month ago? Pain and function. That’s what the health care universe is looking for. Medicare takes it even a step further. They actually state in their documentation guidelines for chiropractors what they want. Unfortunately, this may be one of the best kept secrets in our profession. Medicare actually states that they want us to have the patient complete outcome questionnaires. That means, instead of asking individual questions like “How long can you sit before your butt goes numb?” or “How long can you read before your head feels like it’s
A Failure to Communicate
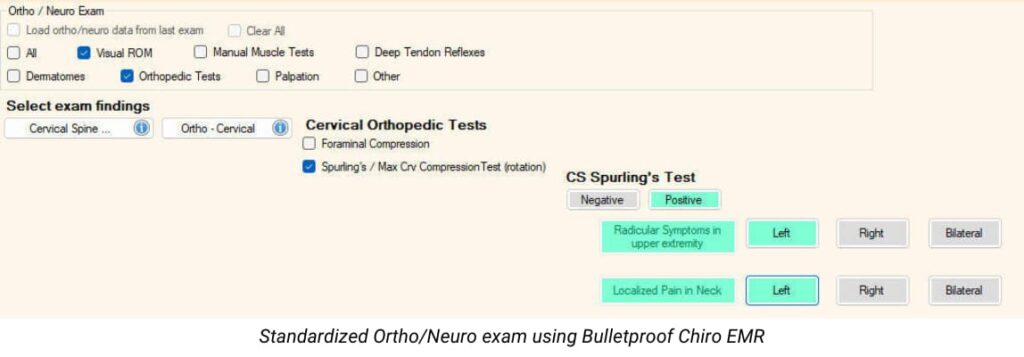
In the old movie, Cool Hand Luke, the Captain said to Luke, “What we’ve got here is failure to communicate.” This has been a major problem with the chiropractic profession since our inception. So many people who’ve never been to a chiropractor have simply no idea what it is that we do and why we do it. In fact, the rest of what I like to refer to as the “Health Care Universe”, which includes other health care providers and payers, has very little understanding of what we do or why we do it. Why not? It’s because of our documentation. How do I put this gently? You see, as a profession, our documentation, um, sucks. I’m a 2nd generation chiropractor and I’ve been treating patients for more than 31 years. I’ve also been reviewing LOTS of records and performing IMEs for quite awhile. If you could see what I see…you might have a better understanding of what I’m talking about. We seem to have little to no standardization of how to perform a history and exam. One patient can go to 10 different chiropractors, and that one patient will likely get 10 different exams, all kinds of different diagnoses and 10 completely different treatment recommendations – some for 2 visits, some for 6 visits and some for a pre-paid package of 53 visits. We’re all over the place, and it makes us, as a profession, look ridiculous. Many chiropractors ask me if they should be sending their patients’ primary care doctor their notes. My answer is always…”NOT IF THEY SUCK.” But, if you document properly, using the “universal” language of healthcare, not language that only chiropractors understand, then, by all means, send the notes. Many chiropractors tend to have a love/hate relationship – hmmm, check that – a hate/despise relationship – with Medicare. What has been our biggest problem with Medicare over the years? Yep – our documentation. Personal Injury? Yeah, the documentation. Blue Cross Blue Shield and other payers? More and more of them are producing guidelines that are putting chiropractors into a full blown panic attack. Why do they keep doing this to us? I suspect it’s because we, as a profession, have done such a poor job of documenting what it is that we do and why we do it. At least that’s a big part of it. So how do we fix it? I can just say “document better,” but that’s too ambiguous. We need to standardize our exams more. We need to address BOTH pain and function, not just pain. Let’s start with the History. Too many chiropractors are taking shortcuts on the history. The standard in the Health Care Universe is the OPQRST method, but we’ve got to ask and document ALL of those letters, and we need to document them for EACH condition that we’ll be treating. We need to understand what the ortho/neuro exam is actually for, and what it’s NOT for. We need to understand how to document the findings of the exam. If I see one more time a chiropractor’s records for a non-radicular patient in which the chiropractor notes Grade 2 muscle weakness, I’m going to spit. We need to wrap our head around using outcome assessments for ALL of our patients. This is not a Medicare thing or a PI thing – it’s a DOCTOR thing. But we need to figure out which outcome assessments are more powerful, take less time and are most cost-effective. We need to accept and embrace some guidelines (I know, a four-letter word, so to speak) that actually HELP us help our patients. The CCGPP Guidelines are an EXCELLENT place to start. We need to know exactly WHEN to re-assess the patient and HOW to determine if our treatment has been effective or not and if we’re justified to continue treating the patient – or not. We need to know exactly when ACTIVE care ends and MAINTENANCE care begins. And, here’s the big one – we need to be able to do ALL of this in the LEAST amount of time, with the LEAST amount of effort (documentation, not the exam or treatment) and, yes, the LEAST amount of cost. Is all of this even possible? You bet it is. But only if we stop failing to communicate. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR

