Sometimes Less is More – A Short Story
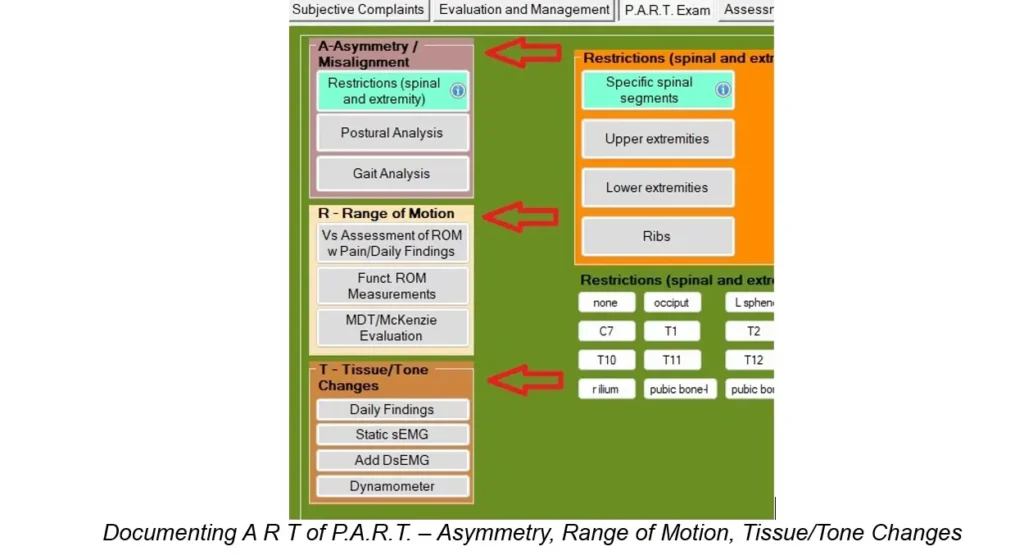
Documentation is a funny thing. For years, chiropractors have been told that our documentation has to “tell the story.” Unfortunately, many chiropractors take that to think they have to write a novel for each patient encounter. The good news is… You may be talking too much. I agree with the premise that we need to tell the story about what is going on with our patients and with each patient encounter. As one who reviews a lot of chiropractic records for insurance companies and attorneys, I can tell you that saying too much does not help. We need to know what parts of the story need to be told. Let’s take our SOAP notes. For the Subjective part, it’s important to document a thorough history on the first visit. The standard for many years has been the OPQRST (onset, provocative/palliative, quality, radiating, site/severity and timing) format, which is required by Medicare. We need to document all of these letters for EACH condition we’ll be treating. On this initial visit, we also need to establish measurable and functional baselines. The key which will make this easier and faster is the use of metrics. Instead of saying “neck pain,” or “moderate neck pain,” we could have the patient rate the intensity of each symptom with the Verbal Numeric Rating Scale (0-10). For more accuracy, we can also have the patient tell us the percentage of their awake time they experience each symptom. Using 5 or 10% increments of time is all we need and is much better than documenting very broad ranges like Occasional, Intermittent, Frequent and Constant. We want to be able to show that the intensity of pain changed from one number to another, and the frequency improved from 95% to 90%, for example. The metrics of intensity and frequency should be documented on every visit. Outcome questionnaires are the part of the story that tells us about the patient’s function. After the first visit, though, we don’t need to be that thorough. All we need to document for the subjective complaints on subsequent visits are the Site, Intensity and Frequency of each symptom, and if the symptom radiates. This should only take SECONDS to document. The outcome questionnaires should be done every 30 days or sooner, according to Medicare, but it’s even better if we re-assess our patients with these questionnaires every two weeks. For our daily “objective” findings, we only need to follow the P.A.R.T. format that Medicare requires. It’s actually really easy to document, so let’s do it for ALL of our patients. We’ve already hit the requirement for the P of P.A.R.T., which is Pain/Tenderness, in the subjective part of our SOAP note. The A of P.A.R.T. stands for Asymmetry/Misalignment, which includes documentation of spinal and/or extremity restrictions (subluxations), posture and gait. If we document the restrictions on every visit, documenting posture and/or gait are optional. All we need to document for the restrictions are the specific segments, like C4, T5 and so on, and left shoulder, right wrist, etc. This should take all of a few seconds to document. No big deal. The “R” of P.A.R.T. stands for Range of Motion Abnormality. If you want to actually measure range of motion (dual inclinometers for spine, goniometer for extremities), this only needs to be done every 30 days. If you want to assess range of motion on each visit, we only need to document if there is an increase in pain or not with each plane of motion. We can also document if there appears to be diminished or restricted motion in each plane, without measuring it or making up a number. The “T” of P.A.R.T. stands for Tissue/Tone. For this, we only need to document muscle spasms and/or trigger points. Instead of documenting the infamous “paraspinal muscles,” though, it’s much better to document the specific muscles, like “left supraspinatus muscle.” That covers the Subjective and Objective part of our S.O.A.P. note. While the metrics for pain intensity and frequency may change on each visit (but not necessarily), the A, R and T of P.A.R.T. may stay the same for a little while. Change them as they change. So, when we think of “telling the story” for each patient encounter, let’s think in terms of a “short story.” Documentation can be easy and exceptional and fast. We just need to know how to justify. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
Documenting Treatment Goals
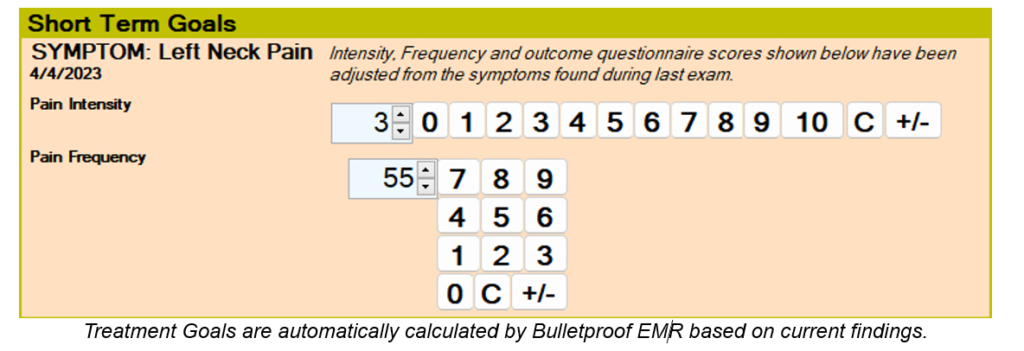
Documenting treatment goals has been an issue for many chiropractors for years. For the few chiropractors who have made the effort, typical goals tend to be things like “reduce pain, reduce muscle spasm, improve range of motion,” regardless of the conditions being treated. When focusing on the Problem Oriented Medical Record format of documentation, which has been the standard since 1968, if we’re treating a patient for headaches, neck pain and low back pain, we should have goals for the headaches, goals for the neck pain and goals for the low back pain. In addition, our goals have to be measurable. In other words, saying “reduce pain” isn’t good enough. We need to say something like, “reduce pain from a 7 to a 5,” or “reduce pain by x%.” Most of you reading this just got nauseous. The next question is, what goals are most relevant to what we do as chiropractors and can be easily calculated and documented? Medicare has been telling us for years that they want to see TWO things from chiropractors: Pain Assessment and Functional Outcome Assessment. It’s not just Medicare who wants this from us now – the entire health-care universe is asking for it, too. And to be perfectly honest, we should be embracing this instead of fearing it. Why? Because we all know how GREAT chiropractic treatment is at improving BOTH pain and function. Why not SHOW it? Let’s talk about pain assessment first. There are quite a few published studies that recommend the Numeric Rating Scale (NRS) and the Visual Analogue Scale (VAS). I’ve used both over the years, and I find the NRS is easier for most patients and doctors. This can be done verbally, as opposed to written (Verbal Numeric Rating Scale [VNRS]). The FREQUENCY of the pain is very often overlooked, though, and is a great metric to track and is easily converted to a goal. This works well when we document the frequency in 5-10% increments of time, such as 25%, 50%, 85%, etc. It does not work well when documenting ranges like Occasional, Intermittent, Frequent and Constant. These two metrics of Pain Intensity and Pain Frequency should be documented for each condition being treated and on every visit. It should only take a few seconds to ask the patient and document their answers. The next metric for the patient’s subjective complaints is the functional outcome assessment. According to CMS (Centers for Medicare and Medicaid Services), this needs to be performed every 30 days or sooner. These work even better if we have the patients complete these every two weeks since it helps us determine quickly if we’re on the right track with the patient or if we need to change the treatment in some way. The fourth metric, which falls under the Objective part of our SOAP note and is optional, are range of motion measurements. Range of motion only serves as an outcome assessment if it’s actually measured, though, not visually estimated by the doctor. This outcome assessment (again, it’s optional), should be performed every 30 days. Just know that the quantity of motion isn’t always clinically relevant. Now that we know which metrics to track (pain intensity, pain frequency, functional outcome questionnaires and range of motion measurements), what should the measurable goals be? According to several published studies, to be considered “clinically significant,” we want to show at least 30% improvement in any of the outcome assessments over a four-week trial of care. You don’t need to show 30% improvement in ALL of the metrics, just one or more. If we’re tracking 3 metrics (pain intensity, pain frequency and functional outcome questionnaires), we have a much better chance of reaching this goal in at least one of these. Some of you are MAD now. “Thirty percent? That’s a LOT!” you may be thinking. It’s not as bad as you think. For example, if the pain intensity is a 7/10, a 30% improvement is a 5/10. Do you think you have a pretty good chance of achieving this within 30 days? If the pain frequency is 80% of awake time, a 30% improvement would be 56% of awake time. If the functional outcome questionnaire score is a 52, a 30% improvement is a 35. As the metrics improve, the 30% mark gets even easier to achieve. For example, if the pain intensity is a 4/10, a 30% improvement is a 3/10 (rounded up from 2.8). See how this works? If you want to figure out a way to calculate these goals manually, it’s certainly doable, but will take a bit of time. This is where technology can help us immensely. In my EMR, I have the program automatically calculate the 30% goal for each metric and it documents it for me. As each metric changes, the goal changes. Chiropractic is awesome. We all know it deep in our souls. Now it’s time to show it. Here are some references you can check out: Younger J, McCue R, Mackey S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep. 2009;13(1):39–43. doi:10.1007/s11916-009-0009-x Clinical versus statistical significance in the assessment of pain relief. Todd KH Ann Emerg Med. 1996 Apr; 27(4):439-41. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM Pain. 2001 Nov; 94(2):149-58. Clinically important changes in acute pain outcome measures: a validation study. Farrar JT, Berlin JA, Strom BL J Pain Symptom Manage. 2003 May; 25(5):406-11. How many repeated measures in repeated measures designs? Statistical issues for comparative trials. Vickers AJ BMC Med Res Methodol. 2003 Oct 27; 3():22. Documentation can be easy and exceptional and fast. We just need to know how to justify. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
Justified
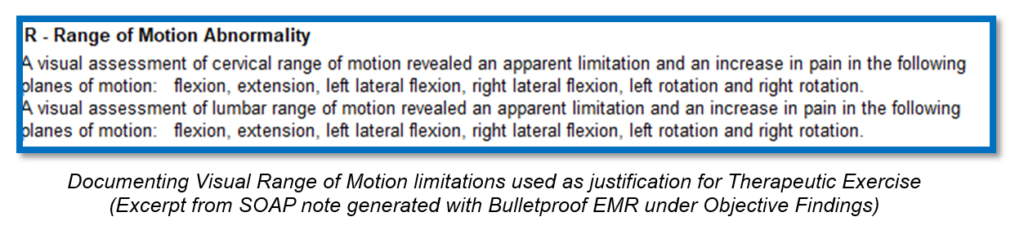
When documenting our Plan, as in what treatment was performed today, it’s important to remember that every form of treatment we provide must be justified by our objective findings. That’s pretty easy when it comes to ice, heat and other passive modalities, like electrical stimulation and ultrasound. Pain and/or muscle spasms are typically enough to justify these modalities. However, the treatments that tend to raise my eyebrows when I review chiropractic records are: Chiropractic Manipulative Therapy Manual Therapy Therapeutic Exercise I’m pretty sure that if I were to ask you what one finding would justify Chiropractic Manipulative Therapy, ALL of you would answer with restriction or subluxation or some other word. Amazingly, though, I’ve been seeing more and more chiropractic records lately in which these are NOT documented. I think there’s an assumption that if you document that you adjusted C3, T4 and L1, it’s obvious that those segments were restricted/subluxated. Don’t assume anything. Let’s start with Chiropractic Manipulative Therapy. If you document in your Plan that C3, T4 and L1 were adjusted, make sure that those segments were noted as restricted/subluxated (other words are OK, too) in your objective findings. The same goes for the extremities. If you adjust the right shoulder, make sure your objective findings reflect a restriction of the right shoulder. So, what about Manual Therapy? This procedure is typically some type of muscle work, so the justification must have something to do with the muscles, such as spasms or trigger points. Stay away from the “paraspinal muscles” when documenting these, though. Be more specific for which muscles, like left trapezius, right levator scapulae, bilateral subscapularis. There’s no requirement to “grade” these spasms or trigger point, so don’t bother wasting your time on that. If you document in your Plan that you performed Myofascial Release, make sure that you name the muscles that were worked on. These same muscles must be noted in your Objective Findings as having spasm or trigger points, though. Make sure you document the amount of time and the reasons why the procedure was performed. How about Therapeutic Exercise? This one has to do with movement, so you’ll want to document which movements/planes of motions the patient was working on, like cervical flexion, cervical left lateral flexion, etc. The justification for this could be as simple as documenting pain in cervical flexion, cervical left lateral flexion, etc. Just like Manual Therapy, make sure you document the amount of time and the reasons why the procedure was performed. Can this be done easily and in very little time? You bet it can. In my EMR, I designed it do this for me. In the Objective Findings part of my SOAP note, I’ll document the spinal and/or extremity restrictions. In the Plan section, I’ll just document spinal/extremity adjustments and my EMR will automatically bring in the specific segments/extremities. When I document the muscle spasms/trigger points in my EMR, I’ll just document Manual Therapy in my Plan and the EMR will automatically bring over the muscles I had already documented in the Objective Findings. When I document pain in various planes of motion in the Objective Findings, I just document Therapeutic Exercises in Plan and the EMR will automatically bring over planes of motion that were previously noted in Objective Findings. Documentation can be easy and exceptional and fast. We just need to know how to justify. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR
It is Complicated
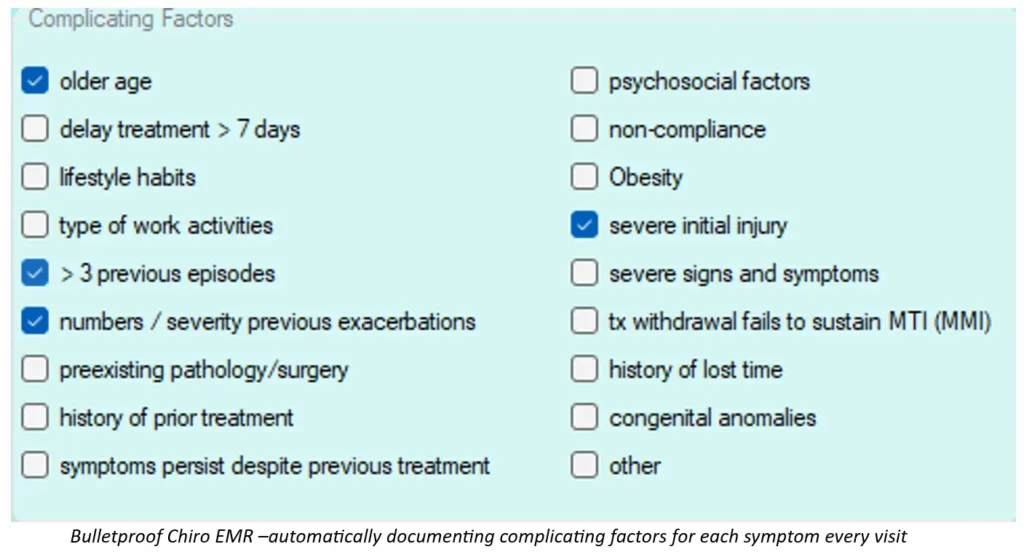
In my previous article, I wrote about how important a great Assessment is in our SOAP notes and how most chiropractors don’t even come close to documenting a good assessment. Some chiropractors complain that some patients respond more slowly than others and that should be taken into consideration. I couldn’t agree more. In fact, a great idea is to document complicating factors for EACH condition you’re treating for each patient, if they exist. A great resource for this is a set of chiropractic guidelines, called Clinical Compass (formerly known as CCGPP). They did all the hard work and found the research to support these. They split up the complicating factors into three categories: Patient Characteristics Injury Characteristics History Patient characteristics include older age, psychosocial factors, delay of treatment > 7 days, non-compliance, lifestyle habits, obesity and type of work activities. Injury characteristics include severe initial injury, > 3 previous episodes, severe signs and symptoms, number/severity of previous exacerbations and treatment withdrawal fails to sustain maximum therapeutic improvement. History includes pre-existing pathology/surgery, history of lost time, history of prior treatment, congenital anomalies and symptoms persist despite previous treatment. I recommend documenting these complicating factors on every visit, just in case your records are ever audited. Medicare, in particular, is notorious for requesting records between “this date” and “that date.” If you don’t have the complicating factors noted on each visit, they may not be present for the dates that are being looked at. And there goes more power out the window. In my EMR, I document any of these complicating factors that exist for each condition on the initial visit. My EMR then has these complicating factors appear on every visit after that – automatically. When documenting the complicating factors in addition to the changing metrics of pain intensity, pain frequency and the outcome assessment scores, your assessment can effectively show how each patient is different and how effective your treatment is, as well as comparing today’s visit to the previous visit. Once we understand and embrace the “rules of engagement,” we can really make our documentation rock. Gregg Friedman, DC, CCSP, FIACA Creator of The Bulletproof Chiro EMR

