Computer-aided Patient Scheduling
Without a computerized scheduler, a practice has less than a 2% chance of earning the title of a “better-performing practice,” according to the Medical Group Management Association. Computerized scheduling helps decrease service costs, provide fairness in service delivery, increase patient satisfaction, and reduce waiting times (Zhang et al., 2019). A massive investment in scheduling features across a wide spectrum of billing products indicates the importance of computerized scheduling. Convenience and front office efficiencies are two obvious benefits of a computerized scheduling system; without them, the only manual way to find out if a specific patient has a scheduled appointment is to flip through the appointment book page by page. Worse, manual scheduling hurts both patient satisfaction and practice financial performance because of scheduling inconsistencies and unbilled (and therefore unpaid) visits. But the benefits of integrated computerized scheduling stretch far beyond convenience, front office efficiencies, and better charge follow-up of stand-alone, albeit computerized, scheduling. A well-designed and integrated scheduler allows preferential patient scheduling, which, along with improved controls, helps revenue optimization and practice compliance. Next, we review key aspects of computerized scheduling and demonstrate the important benefits of integrated scheduling, billing, and compliance management. Scheduling Policies Computerized schedulers allow a combination of single- or multiple-interval scheduling, with open-access scheduling subject to various priority constraints. Such priority-constraint-driven, open-access scheduling creates preferential appointments based on patient demographics or insurance coverage. Typical time-slot-based appointment systems essentially divide a physician’s schedule into finite slots in a day, which can be allocated according to appointment requests. However, such systems are limited by the risks of schedule fragmentations in late shows or no-shows (Chen et al., 2019). Examples of time-slots-based scheduling include single-interval scheduling and multiple-interval scheduling. Single-interval scheduling allocates appointments at regular intervals of 5 to 15 minutes, depending on the specialty. The downside of single-interval scheduling is that as soon as one appointment takes longer than the allocated slot, all subsequent patients must wait. Multiple-interval scheduling also sets appointments at regular intervals; however, unlike single-interval scheduling, it allocates the appointment length depending on the chief complaint. Such scheduling requires up-front categorization of key appointment types and their projected lengths. For instance, an initial appointment might take 30 minutes, while a routine injection might take only 5 minutes. According to the CAHPS survey database, about 12% of patients who called in did not get appointments for urgent care that they needed at the time. Forjuo et al., (2001) also showed that inadequate access to primary care providers was a leading cause of patient dissatisfaction. These challenges are mitigated by open-access scheduling. Open-access scheduling requires holding several appointments open every day. These open appointments are filled only within 48 hours of the appointment, catering to same-day or last-minute patient requests. Open-access scheduling improves access to the physician, reduces no-shows, and eliminates patient screening time. The downside of open-access scheduling is, of course, the potential for longer patient waiting lines or physician idle time because of the inability to maintain a predictable patient flow. A novel scheduling variant is the overlapping appointment scheduling (OLAS) model (Huet et al., 2020). OLAS model refers to deciding the optimal overlapping periods between the patient appointment and allocated service times. The model is formulated as an optimization problem to minimize the total cost of patients waiting and doctors’ idle time. One way to balance the practice workload is to schedule group, routine, or repeat appointments during slow hours. For instance, pediatric well-child visits or patients with a particular chronic disease—such as congestive heart failure or diabetes—could be scheduled for early mornings when there are typically fewer patients waiting in line. These scheduled visits include educational components and often involve multidisciplinary teams. It also helps save time since standard advice need not be repeated to individuals, improving on the efficiency of care delivery (Jones et al., 2019). Patients also benefit from the socialization aspect of group visits; members encourage one another, exercise together, and so forth. A good scheduler allows a repeat appointment schedule subject to total frequency and time slot constraints. Compliance Process An integrated scheduler verifies the filing of a signed patient consent form—and, in certain cases, a signed ABN form. An ABN (Advance Beneficiary Notice) serves three goals: To protect the beneficiaries from liability for services denied as not reasonable (depends on the frequency or duration) and necessary (depends on the diagnosis and the provider’s specialty) To protect the provider’s revenue by shifting financial liability for denied services to the patient To provide documentation for a Medicare audit For more complex procedures, the scheduler warns the front office about the need to obtain all required diagnostic test results and clearances up front. Billing Interface The integrated scheduler avoids unbillable patient encounters and reconciles visits with patient balances. It checks outstanding patient balances and verifies coverage and eligibility at the point of scheduling before the appointment. AI-driven computerized coding and billing systems can accurately provide the code for a particular disease condition and help with appropriate automated billing (Venkatesh et al., 2023). In many cases, such a test discovers data entry errors too, reducing the payment cycle at later stages. Additionally, the insurance company may require referrals or separate pre-authorization/certification for certain procedures, refusing the payment if the procedure was performed without a referral or preauthorization. The integrated scheduler can access medical records to supply necessary background and diagnosis information to obtain pre-authorization. Finally, without the ability to reconcile visits with payments, the practice owner cannot be sure that every visit resulted in a payment. Practice Flow Interface The integrated scheduler manages the entire patient flow, continuously updating arrival lists, checkoffs, and office/room tracking. Further, the scheduler tracks no-shows and follow-up actions. Detailed reports include daily schedules, load reports, missed appointments, free time, canceled appointments, etc. With AI-integrated schedulers, different color codes and status flags can be used for different appointment types, whether emergencies or routine or based on the specialist to be seen by the patient. This offers a good visually appealing summary by just glancing over the
Value Adding for Maximum Profit
I love this topic because it’s easy to miss the mark, especially since so many consultants and marketing firms misappropriate this term and don’t actually coach on value-adding. The idea of value-adding has come under scrutiny in light of the current trend of corporate acquisitions of primary care clinics and the rising patient expectation for comprehensive, patient-centered treatment (Abelson, 2023). This is because of how the healthcare industry is changing. There is a growing need to separate actual value addition from empty rhetoric when corporate companies acquire primary care operations. The demand for genuine, efficient value-adding solutions has never been greater due to the rise in patient expectations for a comprehensive healthcare experience. Don’t get me wrong, plenty do an absolutely amazing job, and their clients see great results, but more often than not, disaster strikes. Especially in the case of Joseph and Bonnie… When Joseph and Bonnie opened their practice, they were die-hard, convinced that they only needed to practice their specialty and nothing else. If we stay true to our specialty’s expertise and principles, we shouldn’t need anything else in the practice to thrive. Although reasonable, this viewpoint failed to consider the changing expectations of healthcare consumers. Patients are increasingly looking for holistic healthcare that covers their current requirements and their long-term well-being, according to Yussof et al. (2022). This suggests Joseph and Bonnie’s single-focused strategy didn’t meet the patient’s desire for comprehensive care. Today’s patients want treatments that address their current health needs and promote wellness, including preventative and long-term health management. Thus, healthcare professionals who offer more services are valued more. So they went about building out a space with the money their mentor had given them and whatever they could find and were adamant that physical therapy was the only service to be offered. Once the space was open, they began marketing to orthopedists in the area and getting patient referrals. That’s when the opportunities opened up. Patients started asking about ancillary services they didn’t have, making them feel like they looked silly. Patients asked about home fitness programs, nutrition, supplementation, and other specialties like Chiropractic or group fitness. The study by Patel & Singhal (2023) demonstrates the growing tendency of patients to seek comprehensive care. It showed that most patients favor healthcare facilities that offer various services under one roof. Patients increasingly view healthcare as a holistic activity. They want nutrition advice, exercise regimens, and alternative cures, not just specialist therapy. This shift in patient preferences fuels the desire for multi-service healthcare facilities that can meet several health and wellness goals. Initially, Joseph and Bonnie ignored it and kept progressing, growing at around 10%. They did a first-quarter review, and it was clear they were not on track to meet their financial freedom goals. They were convinced that something had to change, but they knew working harder to build new referring relationships was not scalable. They could only see so many patients daily, and hiring more therapists would add to their overhead. They needed a solution that minimized overhead growth while maximizing potential revenue. Joseph and Bonnie started taking patient requests seriously and realized a clear pattern. Patients were looking for wellness, not just treatment. Patients wanted to know if they could have a one-stop shop for preventative and therapeutic care. This was a new concept to Joseph and Bonnie, but they began exploring it and found an incredible and vast potential revenue stream in things like product offerings, DME, and more. Such a change toward integrated healthcare delivery is consistent with the ongoing tendency within the pharmaceutical sector to develop into wellness providers with patient-centric services (Moreno, 2019). This represents a larger healthcare shift from treating sickness to promoting well-being. Pharmaceutical corporations are expanding their position to include disease prevention, wellness, and patient-centric services for different health needs. Patients want a single source of preventative and therapeutic care. At first, Joseph and Bonnie only wanted to add what they could manage and keep the specialty singular. However, it soon became clear that their patients were looking for a more sophisticated preventative care so they hired a part-time nutritionist who turned into a full-time nutritionist. They bought used fitness equipment and hired a part-time fitness instructor who turned into a full-time instructor (Joseph recently replaced this person as the full-time trainer because of his personal love of fitness; the perks of being the boss). So what is value adding? Is it simply the addition of multiple complementary specialties into your practice? Maybe. Recent developments in primary and pharmacy care have demonstrated that value addition can be achieved by implementing cutting-edge health methods like digital medicines and remote patient monitoring (Smith, 2021). Value-adding extends beyond incorporating diverse specialties. Digital medicines and remote patient monitoring improve patient care and convenience. These strategies satisfy patients’ desire for individualized, accessible treatment, bringing value to a practice. It could also be the addition of community events, marble floors in the patient bathroom, or a cooling station with fancy refreshments. The true value add in a practice is unique to the patient community. It’s a matter of listening to the value-adds they seek and finding a way to accommodate them that supports the larger purpose and mission. If your practice is in a really nice part of town and you managed to get a great deal on space but are short on cash, it could be a matter of setting up one fancy area in your practice that you can afford to spruce up (it should also be functional, before you go replacing drapes). Whatever change you attempt needs to address two things: Patient requests – Surveys often help the most in this area Patient function – You want the value to add(s) to be usable in some way that improves the patient’s experience both individually and as a group A fancy cooling station with multiple settings, fruit, vegetable-enhanced water, and more can get patients talking and feeling fancy. Often these changes can also help enhance the practice’s
Change Management – Switching Your Billing Systems
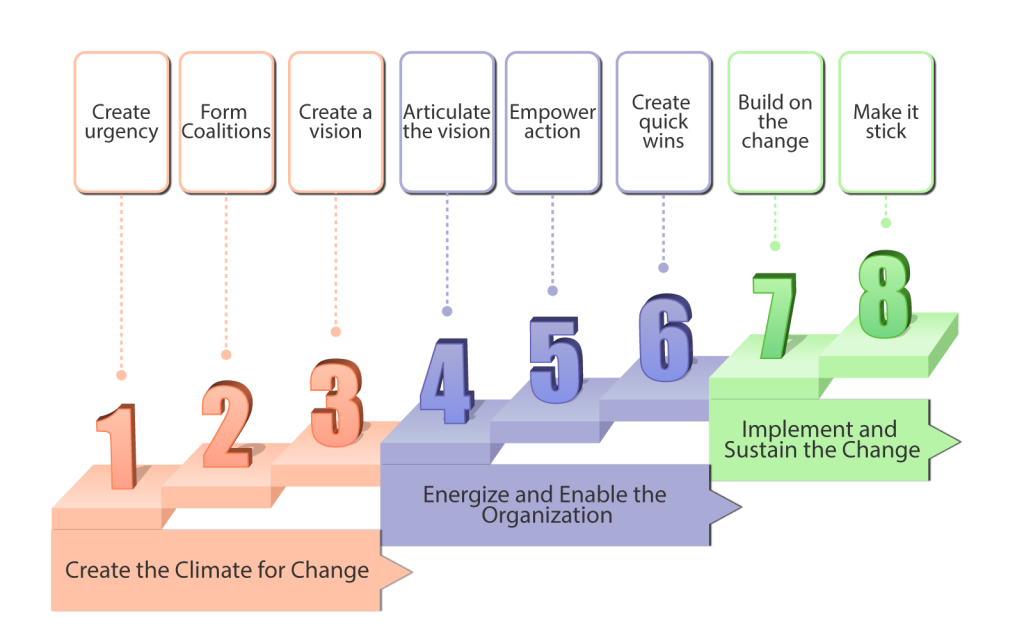
Practice owners seeking better solutions often start with a vision of increased practice profitability while treating reasonable patient volumes. Their vision spans multiple aspects, including better reach to prospective patients, better reimbursement rates, full and timely payments by insurance companies, less time spent on visit documentation, improved documentation quality for better clinical follow-up and lower audit risk, and more free time for family. However, that vision conflicts directly with the payers’ goals to reduce costs and increase revenues. Payers’ goals directly conflict with a provider’s vision because cost savings for payers simply mean that providers treat more patients at lower reimbursement rates—or, in other words, providers work harder for less money. In addition to the basic payer-provider conflict, visionary practice owners must face the resistance of their office managers and colleagues. These people may be skeptical because they don’t trust the owner, have seen five other failed initiatives, or think they might lose something with the change. Significant time, enthusiasm, and resources are needed to change practice processes and technology and to retrain personnel while simultaneously managing the practice and treating patients. The challenge of overcoming resistance to change and implementing it in your practice is akin to enhancing airplane engineering while keeping the plane in the air. Thus, medical practice owners often find themselves in a dilemma between adopting new solutions or compromising the vision and returning to the old ways, along with shrinking revenues and growing frustration. One key area of medical practice that requires a huge transition is shifting from paper-based records to an electronic health record (EHR) system. Shifting from one EHR system to another is also burdensome and requires a systematic approach to achieve results. Several internet-based software and tools can aid medical practices in transitioning to electronic records successfully, leading to maximized outputs and better service delivery to patients. We shall look at how to adopt this change using a change model. EHR and billing processes can help providers cut costs, improve the quality and safety of care, and enhance the productivity of the employees. Most practices have adopted EHR and electronic billing systems to achieve the above goals, whereas some have stuck to using paper documentation and filing systems. Paper-based records are often tiresome to retrieve, prone to errors and misplacements in addition to being bulky and space-consuming to store. Paper-based billing systems have also been shown to take longer claims processing times than EHR due to the time taken to verify manually. To fully realize change and adopt it into practice, a stepwise approach has to be taken, failure to which frustrations and complacencies are bound to occur, leading to regression to previous ways. John Kotter, a Harvard Business School professor and the world’s foremost authority on leadership and change, discovered that transformation challenges span multiple industries and share the same characteristics. His book Leading Change lists an eight-step process for implementing successful transformations. The eight steps can be divided into 3 phases: creating the climate for change, energizing & enabling them, and implementing and sustaining the change (National Learning Consortium, 2013). The figure below illustrates these three phases. Figure 1: The three phases of Kotter’s eight-step change management model This model has successfully been used to help transition into an electronic health records system in clinical practices. For instance, North Shore Medical Center in Chicago, Illinois, successfully transitioned from 100 percent paper-based medical records to 100 percent electronic records in 2013 using Kotter’s eight-step model (Martin and Voynov, 2014). An orthopedic practice group in Ontario, Canada, also successfully transitioned from paper records to electronic records, achieving more than a 95% threshold using Kotter’s change model (Auguste, 2013). We shall look into the eight steps in detail using an example of a healthcare practice that desires to transition from paper-based records to electronic health records and billing. Step 1: Create a sense of urgency. In this step, a health practice can provide evidence to its employees on the need for an EHR. This can include faster claims processing, less bulky storage space, easy records retrieval, and better security. At this stage, the aim is for employees to buy into EHR and keep talking about the proposed change. Step 2: Form a powerful coalition. To help convince employees that change is necessary, the practice can develop a committee of committed and passionate individuals who constantly champion EHR. These individuals can work as a team to help identify barriers to implementation as well as help remind other employees of the need for EHR constantly. Step 3- Create a vision for change. The practice can develop a clear and concise vision through the committee, which motivates transition. An example of a vision would be establishing the most secure health records for clinic patients. Step 4: Communicate the vision for buy-in. Once the vision is created, it must be communicated to the employees clearly explaining the benefits to encourage buy-in. This can be achieved through face-to-face meetings, sending email reminders on the transition from paper to EHR, and individual interviews. Step 5: Remove obstacles. There are 5 categories of barriers hinder any change from occurring in an organization, the biggest of which are complacency and resistance to change (IvyPanda, 2020). The 5 categories include complacency, Limited sharing of the vision, Different obstacles to the vision, Inability to accomplish short-term wins, and failure to solidify the change in the practice culture. Let’s briefly talk about the five categories of barriers. 1. Complacency– This is the most deadly of practice change management problems. Suppose you just plunge ahead with a new electronic medical records (EMR) system or billing process without first establishing a shared sense of immediate need or urgency because of increased audit risk or shrinking revenue. In that case, natural complacency takes over—and the entire change effort fails. It’s hard to drive people out of their comfort zones. Past failures, the lack of a visible crisis, low-performance standards, and insufficient feedback from doctors, office personnel, and patients—all add up to turning the best-intended change initiatives
Maximizing Chiropractic Efficiency: The Power of Integrated Software Solutions
In today’s digital age, the healthcare industry, including chiropractic practices, is rapidly evolving. With the rise of technology, there’s an increasing need for integrated software solutions that can streamline operations, enhance patient experience, and boost overall efficiency. In this context, the integration of platforms like Genesis Chiropractic Software and TrackStat is nothing short of revolutionary. The Need for Automation in Chiropractic Practices Automation is no longer a luxury but a necessity. With the increasing demands on healthcare professionals, manual processes can become tedious and prone to errors. By automating tasks such as patient management, appointment scheduling, and follow-ups, chiropractors can ensure a smoother and more efficient workflow. This not only saves time but also reduces the chances of human error, ensuring that patients receive consistent and high-quality care. Segmentation for Personalized Patient Care One size doesn’t fit all, especially in healthcare. Every patient is unique, with different needs and health conditions. By segmenting patients into different categories based on their health conditions, treatment plans, or other criteria, chiropractors can offer more personalized care. This not only enhances the patient experience but also ensures that each patient receives the most appropriate and effective treatment. The Power of Sales Pipelines in Patient Conversion A robust sales pipeline is crucial for any business, including chiropractic practices. By tracking new patients, their last and next visits, and other relevant information, chiropractors can gain valuable insights into their conversion rates. This data can be instrumental in identifying areas of improvement and implementing strategies to boost patient conversion. Enhancing Patient Retention with Data Analytics Patient retention is a critical metric for any healthcare practice. By analyzing data on patient drop-offs, chiropractors can identify specific points in the patient journey where they’re losing patients. With this information in hand, they can implement targeted strategies, such as educational workshops or progress exams, to enhance patient retention. Streamlining Operations with Two-Way Texting and Smart Reactivations Communication is key in healthcare. Two-way texting allows for seamless communication between chiropractors and their patients, ensuring that patients are always informed and engaged. Additionally, smart reactivations can help chiropractors identify and reach out to patients who haven’t been in for a while, ensuring that they continue to receive the care they need. Reducing Accounts Receivable with Integrated Solutions Financial health is crucial for the sustainability of any practice. By integrating solutions that help reduce accounts receivable, chiropractors can ensure a steady cash flow and financial stability. This not only ensures the smooth running of the practice but also allows chiropractors to invest in further enhancing their services. Conclusion The integration of platforms like Genesis Chiropractic Software and TrackStat offers a plethora of benefits for chiropractic practices. From automating tasks to enhancing patient experience and boosting efficiency, these integrated solutions are truly game-changers. As the healthcare industry continues to evolve, it’s crucial for chiropractors to leverage the power of technology to stay ahead of the curve and offer the best possible care to their patients. Note: For a deeper dive into these topics and to hear firsthand experiences from industry experts, watch the video at the top of this page.

