ClinicMinders make our company what it is. We hire for attitude over experience and we pride ourselves on attracting and retaining people with COURAGE.
COURAGE to stick to our Core Values and help providers remain independent and grow. We also believe in radical transparency, so we publicly share Core Values with anyone who is interested in our approach to work. This fanatical focus is more than a mantra; it is evident in our software, our support, and the services we keep adding. And doing so makes us ecstatic.
ClinicMind offers great benefits, an attentive team, and a flexible and professional work environment
ClinicMind offers a work-from-home (WFH) employment structure for work-life balance and professional growth. WFH benefits promote job satisfaction, family focus, and productivity.
ClinicMind leverages its access to the global talent pool and fosters a strong remote company culture through adherence to the core values of excellence, learning, and teamwork.

ClinicMind is a health technology company delivering comprehensive EHR, RCM, and practice management solutions. Our mission is to empower healthcare providers. Mainly chiropractors with intuitive, scalable, and compliant technology that simplifies workflows, enhances patient outcomes, and maximizes revenue cycle efficiency.
Position Summary:
The Chief Chiropractic Officer (CCO) will serve as the strategic and clinical leader for chiropractic initiatives at ClinicMind. This executive will shape the company’s vision and direction for chiropractic care, guide the development of chiropractic-specific technology solutions, and represent ClinicMind within the broader chiropractic profession.
Key Responsibilities:
Strategic Leadership: Define and drive ClinicMind’s vision for the chiropractic profession, ensuring alignment with market trends, regulatory changes, and future innovation.
Product Influence: Partner with product and engineering teams to guide the development of next-generation chiropractic EHR and practice management software.
Clinical Oversight: Ensure clinical relevance, compliance, and usability of chiropractic-specific features in ClinicMind’s platform.
Thought Leadership & Advocacy: Actively participate in chiropractic associations, conferences, publications, and key industry events as a ClinicMind representative.
Education & Mentorship: Serve as a voice and mentor for the next generation of chiropractors through educational initiatives, webinars, and community engagement.
Market Insight: Monitor competitive landscape and identify opportunities to improve ClinicMind’s positioning and services for chiropractic professionals.
Collaboration: Work cross-functionally with the CEO, CTO, Marketing, Product, and Sales teams to ensure chiropractic users’ needs are met and exceeded.
Must-Have Skills & Qualifications:
Vision for the Chiropractic Profession: Proven ability to define, articulate, and lead strategic direction for chiropractic care in a digital environment.
Industry Engagement: Demonstrated history of active participation in major chiropractic associations, national/international events, and published contributions in respected journals or media.
Technology Proficiency: Strong understanding of practice management and EHR systems, especially in relation to office workflow and compliance.
Leadership in Software Evolution: Deep interest and capacity to influence the future of chiropractic software through direct product feedback and innovation.
Doctor of Chiropractic (DC) degree and current or prior licensure required.
10+ years of clinical chiropractic experience, with at least 3–5 years in leadership, advisory, or health tech roles preferred.
What We Offer:
Opportunity to lead innovation in the chiropractic profession on a national scale
A collaborative, mission-driven environment at the intersection of healthcare and technology
Competitive executive compensation
Flexible remote working arrangement
The chance to directly impact how chiropractors deliver care and manage their practices
ClinicMind’s core values—Excellence · Learning · Teamwork guide everything we build.
With 150 in‑house analysts, half a dozen BPO partners, and a proprietary billing platform, we now need a manager to deliver best‑in‑class collections, continue to improve performance, automate, and meet the RCM needs of a rapidly growing client base.
Position Summary:
The RCM Aging Manager is responsible for overseeing the resolution and collection of aged medical insurance claims to ensure timely and accurate reimbursement. This role leads a team of billing and follow-up specialists focused on reducing outstanding accounts receivable (AR), identifying root causes of claim denials or delays, and implementing process improvements to prevent future aging. The manager serves as the key liaison between billing staff, payers, and internal departments to enhance claim performance and cash flow.
Key Responsibilities:
Leadership & Oversight
Supervise a team of billing and collections specialists handling aged or unresolved insurance claims.
Assign workloads, set performance goals, and monitor productivity and quality metrics.
Conduct regular team meetings to review AR status, payer trends, and action plans.
Provide training, mentorship, and performance evaluations for team members.
Claims Management & Resolution
Oversee the daily review and follow-up of aged insurance claims (commercial, government, PIP, workers’ comp, and other third-party payers).
Ensure appropriate actions are taken on denied, underpaid, or unpaid claims.
Develop and implement work queues, escalation procedures, and aging reports to prioritize collection efforts.
Collaborate with payers to resolve complex or disputed claims and obtain proper reimbursement.
Monitor timely filing limits and ensure corrective actions are completed before claims are at risk of write-off.
Data Analysis & Reporting
Analyze AR aging reports to identify trends, bottlenecks, and payer-specific issues.
Prepare weekly and monthly performance reports, including recovery rates, claim volumes, and aging metrics.
Track key performance indicators (KPIs) such as AR days, denial rates, and collection effectiveness.
Recommend process improvements to streamline claims management and reduce aging inventory.
Compliance & Quality Assurance
Ensure billing and follow-up activities comply with federal, state, and payer-specific regulations.
Maintain adherence to HIPAA and organizational privacy/confidentiality standards.
Partner with compliance and quality teams to correct systemic billing or coding issues.
Collaboration & Communication
Work closely with coding, billing, and denial management teams to resolve issues impacting aged claims.
Communicate with internal departments to gather documentation or clarification necessary for claim resolution.
Represent the department in meetings related to payer performance and AR reduction strategies.
Qualifications:
Education:
Associate’s or bachelor’s degree in business administration, Healthcare Management, or related field preferred.
Equivalent combination of education and experience may be considered.
Experience:
5+ years of experience in medical billing, claims follow-up, or insurance collections.
2+ years of supervisory or management experience within a healthcare billing or revenue cycle environment preferred.
Strong understanding of payer rules, EOBs, denial management, and reimbursement methodologies.
Skills & Competencies:
Deep knowledge of medical billing and insurance claim processes.
Proficiency in billing systems and electronic health record (EHR) software.
Strong analytical and problem-solving skills.
Excellent communication, leadership, and team management abilities.
High attention to detail and organizational skills.
Performance Metrics:
Reduction in aged AR (especially >120 days).
Increased collection rates and decreased denial ratios.
Team productivity and claim resolution turnaround time.
Compliance with payer and regulatory guidelines.
Staff engagement and retention within the department.
Must Have:
ClinicMind’s core values—Excellence · Learning · Teamwork guide everything we build.
With 150 in‑house analysts, half a dozen BPO partners, and a proprietary billing platform, we now need a manager to deliver best‑in‑class collections, continue to improve performance, automate, and meet the RCM needs of a rapidly growing client base.
Position Summary:
The RCM AR Follow-Up Manager oversees the daily operations of the Accounts Receivable team responsible for timely follow-up and resolution of billed medical insurance claims. This role ensures that outstanding claims are pursued, denials are addressed promptly, and payments are collected efficiently to maintain optimal cash flow and reduce aged receivables. The manager serves as the liaison between the AR staff, billing team, payers, and leadership to ensure compliance, productivity, and accuracy in all AR activities.
Key Responsibilities:
1. Leadership and Oversight
Supervise, train, and mentor a team of AR follow-up specialists and lead representatives.
Assign workloads, monitor productivity, and track key performance indicators (KPIs) such as Aging and claim resolution rate.
Conduct regular team meetings to discuss performance, process improvements, and payer updates.
Foster a positive, accountable, and results-driven team culture.
2. AR Management
Oversee the timely and accurate follow-up on all unpaid, underpaid, and denied insurance claims across all payer types.
Ensure all claims are followed up in accordance with payer timely filing limits.
Monitor and analyze aging reports to identify trends, payer issues, and root causes of delays.
Work closely with the billing and cash posting teams to reconcile discrepancies and resolve claim-related issues.
3. Process and Performance Optimization
Develop and implement policies, procedures, and workflows to streamline AR operations.
Evaluate and improve claim follow-up strategies to enhance collections and minimize rework.
Utilize reports and dashboards to track team performance and identify improvement opportunities.
Collaborate with IT or system administrators to optimize billing software tools and automation.
4. Payer and Denial Management
Maintain strong relationships with insurance representatives to expedite claim resolution.
Oversee the research and resolution of complex claim denials and payment variances.
Provide feedback to billing and coding teams on denial trends and documentation needs.
Ensure appeals are filed accurately and timely with proper documentation and justification.
5. Compliance and Quality Assurance
Ensure all AR activities comply with HIPAA, payer contracts, and company policies.
Maintain confidentiality of patient information and financial data.
Conduct periodic quality audits to ensure accuracy in claim follow-up and note documentation.
Stay current with payer regulations, policy changes, and industry best practices.
6. Reporting and Communication
Prepare and present weekly, monthly, and quarterly AR performance reports to senior management.
Communicate collection trends, issues, and successes across the revenue cycle leadership team.
Recommend actionable strategies to reduce days in AR and improve cash flow.
Qualifications:
Education:
Associate’s or bachelor’s degree in business administration, Healthcare Management, or related field preferred.
Equivalent combination of education and experience may be considered.
Experience:
5+ years of progressive experience in medical billing, AR follow-up, or revenue cycle management.
2+ years in a supervisory or management role overseeing AR or collections teams.
Strong knowledge of payer policies, denial management, and reimbursement methodologies (commercial, Medicare, Medicaid, PIP, workers’ comp, etc.).
Skills & Competencies:
Proficiency in billing systems and electronic health record (EHR) software.
Advanced Excel and data analysis skills.
Strong leadership, coaching, and team-building abilities.
Excellent problem-solving, analytical, and organizational skills.
Clear communication and negotiation skills with internal staff and payer representatives.
Ability to manage multiple priorities in a fast-paced environment.
High attention to detail
Performance Metrics:
Days in AR (goal: maintain below industry benchmark)
AR >90 days percentage
Denial rate and resolution rate
Cash collections to net revenue ratio
Team productivity (claims followed up per day)
Timeliness and accuracy of claim follow-up documentation
Must Have:
ClinicMind’s core values—Excellence · Learning · Teamwork guide everything we build.
With 150 in‑house analysts, half a dozen BPO partners, and a proprietary billing platform, we now need a manager to deliver best‑in‑class collections, continue to improve performance, automate, and meet the RCM needs of a rapidly growing client base.
Position Summary:
The PIP Insurance Billing Manager oversees and manages all aspects of the Personal Injury Protection (PIP) billing process. This position is responsible for ensuring timely and accurate submission of PIP claims, managing a team of PIP billers and follow-up specialists, and ensuring compliance with all state-specific insurance laws, payer requirements, and internal policies. The manager works closely with attorneys, patients, providers, and insurance adjusters to resolve claim issues and maximize reimbursement.
Key Responsibilities:
Leadership & Oversight:
Supervise, train, and mentor a team of PIP billers and collection specialists.
Assign and monitor daily workloads to ensure timely and accurate billing and follow-up on all PIP claims.
Conduct regular performance evaluations, provide coaching, and implement process improvements to enhance team productivity.
Foster a positive and collaborative work environment.
Billing & Claims Management:
Oversee the preparation and submission of all PIP claims, ensuring accuracy and compliance with state-specific requirements.
Review and approve adjustments, write-offs, and appeals to ensure they align with company policies and payer guidelines.
Monitor claim status reports and follow up on unpaid, underpaid, or denied PIP claims.
Ensure proper coding (ICD, CPT, HCPCS) and documentation for all submitted claims.
Compliance & Quality Assurance:
Stay current with state PIP laws, no-fault insurance requirements, and payer policies.
Ensure that all billing practices are compliant with federal, state, and payer-specific regulations.
Develop and implement standard operating procedures (SOPs) for PIP billing and collections.
Conduct periodic internal audits to identify and correct billing errors or compliance risks.
Reporting & Analysis:
Generate and analyze billing, collections, and aging reports for PIP accounts.
Track performance metrics including days in A/R, denial rates, and reimbursement trends.
Provide regular updates and strategic recommendations to leadership regarding PIP collections performance.
Collaboration & Communication:
Serve as the primary liaison between billing staff, clinical teams, attorneys, and insurance carriers.
Work with providers and medical records departments to ensure timely receipt of necessary documentation.
Qualifications:
Education:
Associate’s or Bachelor’s degree in Business Administration, Healthcare Management, or related field preferred.
Equivalent combination of education and experience may be considered.
Experience:
Minimum 3–5 years of experience in PIP billing or no-fault insurance claims required.
Strong understanding of state-specific PIP and no-fault laws.
Skills & Competencies:
Deep knowledge of insurance billing, reimbursement processes, and medical terminology.
Excellent leadership, communication, and problem-solving skills.
Strong analytical and organizational abilities with attention to detail.
Proficiency in Microsoft Office Suite (Excel, Word, Outlook).
Ability to work under pressure, meet deadlines, and manage competing priorities.
Performance Indicators:
Accuracy and timeliness of PIP claim submissions.
Reduction in claim denials and days in accounts receivable.
Team productivity and morale.
Compliance audit results.
Overall recovery rate of PIP reimbursements.
Must Have:
The SuperPool Team Lead (TL) will oversee a group of Onboarding Account Managers (OAMs) while also directly managing a portfolio of client accounts. The TL ensures adherence to ClinicMind’s Onboarding Lifecycle, provides coaching and support to OAMs, and maintains accountability for client satisfaction, efficiency, and successful go-lives.
This role requires balancing leadership responsibilities with hands-on client management, acting as both a coach and role model for the team.
Key Responsibilities
Team Leadership
Required Skills & Qualifications
Key Competencies for Success
As a Senior GoHighLevel Developer, you will lead the design, development, and optimization of automation and integration workflows within ClinicMind’s environment. A critical part of this role involves implementing robust tracking and reporting mechanisms to measure the effectiveness of all GHL-driven initiatives. You’ll customize GHL to meet healthcare-specific needs, connect it with internal systems and third-party platforms, and ensure all automations are efficient, scalable, and HIPAA-compliant.
This is a highly collaborative, hands-on role ideal for a developer passionate about technology, automation, and data-driven optimization. You’ll work with teams across engineering, product, marketing, and operations to enhance automation reliability, provide actionable performance insights, and optimize patient journeys and business workflows.
Key Responsibilities
Architect, design, and implement advanced workflows, pipelines, and triggers within GoHighLevel.
Customize funnels, forms, scheduling systems, and automated communication sequences for patient engagement.
Integrate GHL with ClinicMind’s EHR, billing, CRM, and marketing systems via APIs and webhooks.
Develop and maintain custom scripts, functions, and automation logic for secure data handling.
Design, implement, and maintain custom reporting structures, dashboards, and analytics within GoHighLevel to provide key performance indicators (KPIs) on patient engagement, funnel conversion, and communication efficacy.
Troubleshoot and optimize automations for reliability, deliverability, and scalability.
Ensure compliance with HIPAA and healthcare data privacy regulations.
Document all workflows, integration logic, and best practices.
Collaborate with cross-functional teams to translate business needs into automation solutions.
Develop and execute data synchronization strategies between GHL, our EHR/CRM systems, and BI tools to ensure a single, accurate source of truth for all automation and patient data.
Mentor and support junior developers or automation specialists on GHL best practices.
Required Qualifications
5+ years of hands-on experience in automation development in GoHighLevel (GHL), including deep expertise in GHL’s reporting features, custom values, and data aggregation for performance measurement.
Proven experience with API integrations (REST, JSON, Webhooks).
Proficiency in JavaScript, HTML, and CSS for front-end customization.
Hands-on experience with Twilio, Mailgun, and other communication APIs (SMS, email, voice).
Familiarity with Zapier, Make (Integromat), Pabbly, or similar middleware tools.
Strong problem-solving, debugging, and documentation skills.
Excellent collaboration and communication skills in a remote, cross-functional environment.
Solid understanding of healthcare workflows, data handling, and patient engagement principles.
Qualifications
Experience in healthcare IT, EHR, or medical billing systems.
Knowledge of HIPAA compliance and data security standards.
Experience with white-label or multi-account GHL setups.
Exposure to serverless automation tools (AWS Lambda, Google Cloud Functions).
Familiarity with database integrations (MySQL, Firebase, Airtable, etc.).
Prior experience in agency or marketing tech environments.
Position Requirements
Must have a stable internet connection minimum of 25 MBPS
Must have a mobile data plan as a backup
Must be in a quiet environment / work from home set-up
Must be comfortable working the US Eastern Time business hours
Minimum system requirement: Latest i5 with SSD hard disk (i7 preferred), 16GB RAM (32 GB preferred)
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, is looking for a full-time Credentialing Specialist. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
RESPONSIBILITIES
Handle credentialing needs for our clients (Group and/or Individual) who are US-based health care providers, diagnostic laboratories and medical facilities as preferred providers in health care networks. This entails the following tasks:
QUALIFICATIONS
MUST HAVE:
ClinicMind is a leader in providing innovative solutions for healthcare practice management, delivering tools that empower clinics to run more efficiently while enhancing patient engagement. Our PatientHub platform enables seamless communication, scheduling, and interaction between patients and providers.
We are seeking a highly skilled Support Specialist to join the PatientHub Team within our Service Delivery division. This is a client-facing role that requires strong technical knowledge, excellent communication skills, and the ability to troubleshoot and guide customers effectively in a fast-paced, tech-driven environment.
Responsibilities
Serve as the first point of contact for PatientHub clients, providing professional, empathetic, and timely support.
Troubleshoot, diagnose, and resolve issues related to the PatientHub platform and integrated technologies.
Handle Level 2 support responsibilities, taking ownership of escalated technical issues that require deeper investigation and resolution.
Perform advanced troubleshooting and work cross-functionally to coordinate resolutions across multiple teams.
Leverage GoHighLevel expertise to configure, optimize, and support client workflows.
Assist clients in adopting and effectively using AI and Machine Learning technologies within PatientHub.
Document and escalate technical issues to the appropriate teams when necessary.
Collaborate cross-functionally with the Service Delivery division to ensure a seamless client experience.
Educate clients on system best practices, including communication, scheduling, and engagement tools.
Maintain accurate and detailed records of client interactions and resolutions.
Stay current on updates, tools, and best practices relevant to PatientHub, GoHighLevel, and industry trends.
Qualifications
Fluent English communication skills (both written and verbal) are required.
2+ years of hands-on GoHighLevel experience (certification strongly preferred).
3+ years of customer service experience in a client-facing environment.
Experience working with Machine Learning / AI technology.
Strong problem-solving skills and the ability to manage multiple tasks effectively.
Demonstrated ability to work independently in a remote setting.
Experience with websites and SEO is a plus, though not required.
Must Have
Reliable broadband internet connection and a dedicated, quiet workspace for remote work.
High comfort level working on Eastern Time Zone/US Shift
Laptop/Desktop with at least 16 GB
We are a Health IT and RCM service company with a leading-edge EHR software product and a medical billing BPO. We are looking for an enthusiastic Sales Development Representative. If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
Responsibilities:
Demonstrate basic functionality of our product.
Identify potential clients and generate new business opportunities for the company
Cold call potential clients to generate interest in our products and services
Send out personalized emails and LinkedIn messages to potential clients to nurture leads
Monitor appropriate social media groups/communities for potential leads
Schedule appointments with potential clients for the sales team
Provide accurate and up-to-date information on our products and services to potential clients, and this includes product and service demonstrations using presentation materials
Work with the sales team to develop strategies for lead generation and follow-up
Track progress towards meeting sales goals
Collaborate with the sales team to develop strategies for reaching sales targets
Use customer relationship management (CRM) software to manage leads and sales activities
Stay up-to-date on market trends, competition, and industry developments
Provide regular reports on sales activities and results to management.
Qualifications:
2-3 years of experience in sales.
Bachelor’s degree in business or related field
Experience in the healthcare industry preferred but not required
Excellent verbal and written communication skills
Ability to work in a fast-paced environment and handle multiple priorities
Strong interpersonal skills and ability to build relationships with potential clients
Self-motivated and goal-oriented
Proficient in Microsoft Office and CRM software
Position Requirements
Must have stable internet connection minimum of 5 MBPS
Must have a mobile data plan as a backup
Must be in a quiet environment
Must be comfortable working the US business hours
Must own a PC with at least 8 GB of memory
ClinicMind, the nation’s leader in multi-specialty Electronic Healthcare Records (EHR) software and Revenue Cycle Management (RCM) services, is looking for a full-time Video Editor . If you’re excited to be part of a winning team, ClinicMind is a perfect place to get ahead.
At ClinicMind, we are at the forefront of innovation, developing cutting-edge software solutions that empower businesses and individuals worldwide. Our dynamic team thrives on creativity, collaboration, and a passion for excellence. We are seeking an experienced, creative, and innovative Video Editor to join our growing team and help us create engaging and compelling video content that tells our brand’s story.
Key Responsibilities:
As a Video Editor at ClinicMind, you will play a pivotal role in crafting high-quality video content that resonates with our audience. You will work closely with our marketing, product, and design teams to produce a variety of video materials, including explainer videos, promotional videos, tutorials, social media content, and more. Your keen eye for detail, creative storytelling ability, and technical expertise will be essential in delivering videos that align with our brand’s vision and objectives.
Collaborate with the marketing and product teams to understand project requirements and objectives.
Develop creative ways to put our content into a visually appealing story.
Edit raw footage into polished, high-quality videos that effectively communicate our message.
Implement creative techniques, including motion graphics, visual effects, storyboards, and sound design, to enhance video content.
Ensure consistency and alignment with brand guidelines and visual identity.
Manage multiple projects simultaneously, adhering to deadlines and maintaining high standards of quality.
Stay up-to-date with healthcare and technology trends, tools, and technologies to continually improve video production processes.
Provide creative input and suggestions to enhance video concepts and storyboards.
Troubleshoot technical issues and ensure optimal video quality for various platforms (web, social media, etc.).
Maintain an organized archive of video assets and project files.
Qualifications:
At least 5 years experience as a Video Editor, preferably within a software or technology-focused company.
Proficiency in video editing software such as Adobe Premiere Pro, Final Cut Pro, After Effects, or similar tools.
Strong understanding of video production processes, including pre-production, shooting, and post-production.
Excellent storytelling skills with a keen eye for detail, innovative aesthetics.
Ability to work independently and collaboratively in a fast-paced, deadline-driven environment.
Strong communication skills and the ability to effectively present ideas & concepts.
Knowledge of motion graphics, animation, and visual effects is a plus.
Familiarity with audio editing and sound design is an advantage.
Bachelor’s degree in Film, Media, Communications, or a related field, or equivalent work experience.
MUST HAVE:
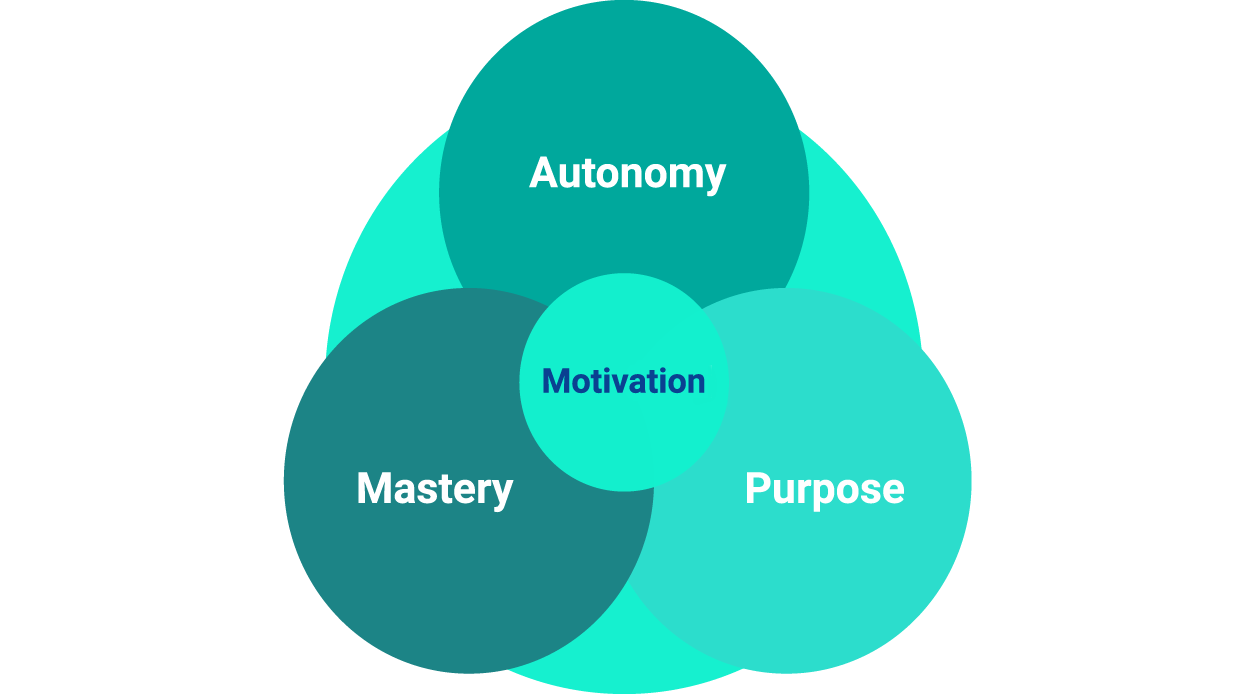
We strive for excellence throughout our hiring process.
We share the purpose of making a lasting change in the healthcare industry by building together state-of-the-art software and using it to level the playing field with the payers.
We invest our energies in learning and mastering our skills, and we grow our responsibilities in step with our professional and business growth.
This site includes cumulative user rating numbers, video testimonials, press releases, and other social proof materials across all brands and all resellers leveraging ClinicMind Software and/or Service as a Platform (SaaP). For more detail about our white labeling and reselling models, visit our About Page or Contact Us directly. Check Privacy Policy