Hear What Our Clients Have to Say
See why healthcare providers trust us to simplify credentialing and elevate their professional journeys.

With our secure document database and credentialing e-documentation, managing your credentials has never been easier. Plus, we handle payer communication on your behalf while ensuring compliance, verification, and ease of setup.
We streamline credentialing for: ✅ Individual providers & group practices ✅ Clinics,DME suppliers, and specialty facilities ✅ Provider database collection & committee review to ensure compliance
We ensure compliance with industry regulations for all payer credentialing requirements. ✔ Medicare & Medicaid ✔ All major commercial plans ✔ Managed care (HMOs, PPOs) ✔ State & federal healthcare programs
📞 Talk to a credentialing expert today! Let’s build a plan that fits your needs
💡 Looking for bundled pricing? Select multiple services & save!
💬 Have questions about the process? Check out our Credentialing FAQ for quick answers!
After signing your contract, we kick things off with a welcome call where you’ll meet your credentialing team and walk through the entire process—so you know exactly what to expect.
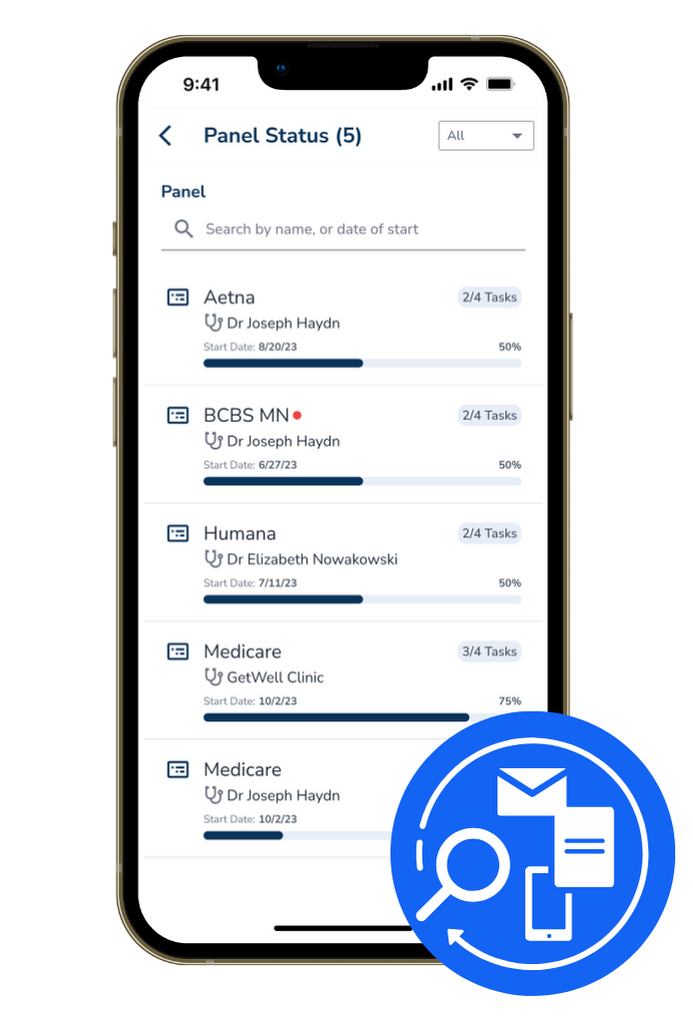
Using the CredEdge Credentialing App, you’ll enter and upload the required information to complete applications. Our secure e-Documentation system ensures that all your credentialing files are stored, verified, and ready for submission. No more missing documents or last-minute scrambling—we maintain everything in one place for you.
✅ We handle submissions and track your applications with payers.
✅ You get real-time updates—log into the Credentialing App anytime to check your status.
✅ We manage follow-ups, respond to payer requests, and keep you informed with weekly updates.
Once your applications are approved, we keep your credentials up to date by managing:
✔ Renewals & re-enrollments
✔ Updates to CAQH & PECOS accounts
✔ Compliance tracking to maintain eligibility
✔ Instant notifications on application status updates
✔ Easy access to all credentialing documents in one place—licenses, insurance, NPI details, and more
✔ Seamless communication with our team—see real-time updates and notes from our credentialing specialists
See why healthcare providers trust us to simplify credentialing and elevate their professional journeys.
This site includes cumulative user rating numbers, video testimonials, press releases, and other social proof materials across all brands and all resellers leveraging ClinicMind Software and/or Service as a Platform (SaaP). For more detail about our white labeling and reselling models, visit our About Page or Contact Us directly. Check Privacy Policy
Credentialing mistakes and delays could be costing your practice thousands in lost reimbursements.
Get a free credentialing evaluation from our experts to identify inefficiencies, prevent costly errors, and ensure your providers get credentialed and paid—faster.